Management
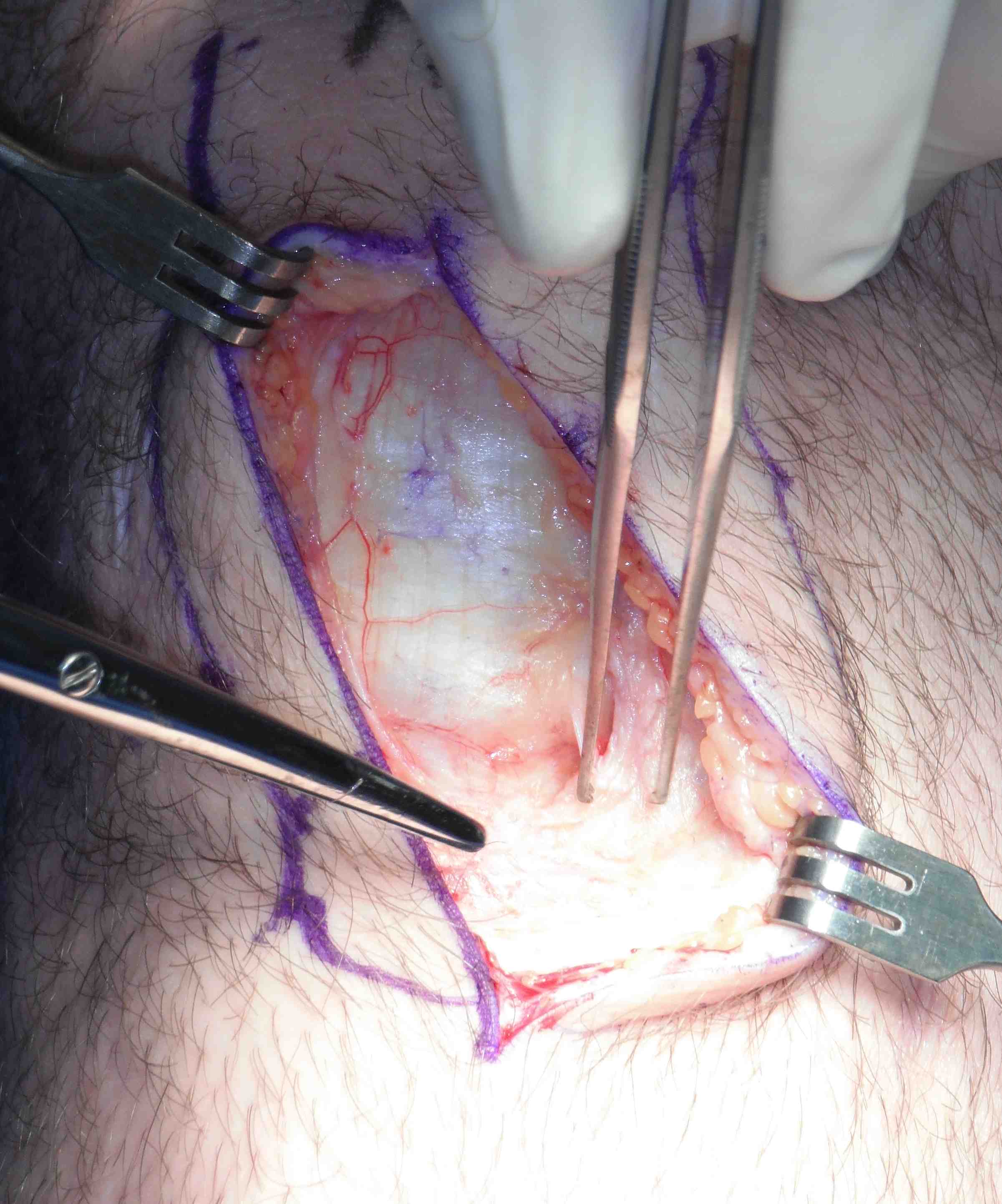
Operative management
Options
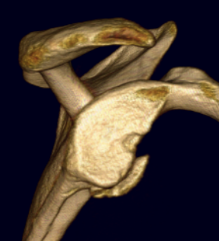
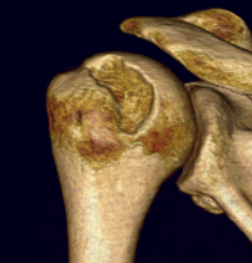
Arthroscopic labral repair +/- Remplissage
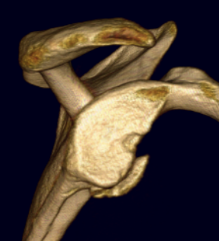
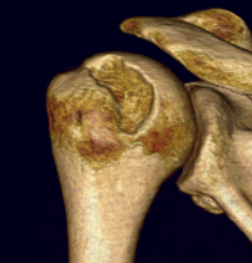
Arthroscopic labral repair +/- Remplissage

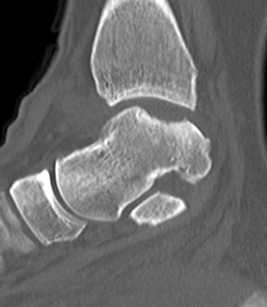
Defect of cartilage +/bone
Typically on talus
Indication
Bony defects > 30 %
Options
- Latarjet - may be insufficient for lesions in the region of 50%
- Iliac crest - associated with high incidence of OA
- distal tibial allograft - radius of curvature matches glenoid highly
Bone healing requires 3 things
- osteoconduction - scaffold / matrix
- osteoinduction - growth factors
- osteogenesis - cells to produce osteoid
Definition
- property of a matrix that supports the attachment of bone forming cells for subsequent bone formation
Substances
1. Isolated LCL injury
2. Isolated Posterolateral Corner
3. PCL + posterolateral corner
4. ACL / posterolateral corner
5. ACL / PLC / posterolateral corner
Levy et al. Am J Sports Med 2010
- failure in 4/10 knees treated with acute primary repair
Harvest graft


Good initial results but unacceptably high failure rate with longer follow-up
Problems
1. Too stiff (low ultimate strain)
- poor resistance to abrasion
- ligament failure by attrition most common
2. Recurrent synovitis, infection, loosening and osteolysis