Operative Management of Humeral Shaft Fractures
Options
Open ORIF with plate
MIPO
Intra-medullary nail
Evidence
Nail v plate
Beeres et al. Eur J Trauma Emerg Surg 2021
- IM nail v open plate
- meta-analysis of 10 RCTs (500 pts)
- SR of 18 observational studies (4900 pts)
- 17% of IMN required reoperation for shoulder impingement
- IMN had faster union and lower infection rate
- no difference nonunion rates or shoulder function scores
van der Wall et al. Eur J Trauma Emerg Surg 2021
- IM nail v MIPO
- meta-analysis of 2 RCTs (87 pts)
- systematic review of 5 observational studies (600 patients)
- MIPO lower risk of nonunion and re-intervention
- MIPO better shoulder function
ORIF v MIPO
- MIPO v ORIF
- meta-analysis of 2 RCTS (98 pts)
- systematic review of 7 observational studies (263 patients)
- MIPO lower risk of nonunion
- no difference in infection or time to union
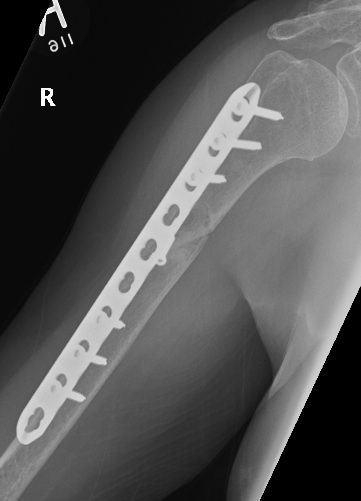
Open ORIF with plate

Approaches
Anterolateral approach - proximal 2/3 of humerus
Posterior approach - distal 1/3 of humerus
- triceps split
- paratricipital - posterolateral approach / posteromedial approach
- triceps flip
Anterolateral Approach Humerus for proximal / mishaft fractures



AO foundation surgical approach
Indication
- proximal fractures
- midshaft fractures
Set up
- lazy beachchair
- flat with arm on arm table
- ensure can get good images of humeral head
Incision
- deltopectoral proximally (to coracoid)
- lateral humerus distally
- distally between mobile wad and biceps
Proximally
- deltopectoral groove
- identify and protect cephalic vein
- take vein laterally to minimis bleeding
- can partially release deltoid insertion if needed
Distally
- follow cephalic
- open fascia laterally
- identify plane between biceps and brachialis
- biceps swept medially
- protect musculocutaneous nerve between the two
- will emerge as lateral cutaneous nerve of the forearm distally
- identify and split brachialis in midline
- can reflect brachialis medially, but will potentially damage radial innervation of medial brachialis
Distal extension
- between brachialis and brachioradialis in distal 1/4
- find and protect radial nerve as it emerges anteriorly through lateral intermuscular septum
- may be easiest to find radial nerve most distally between brachialis and bradioradialis
- avoid lateral hohman retractors in this area
Internervous plane
- radial nerve lateral brachialis
- musculocutaneous nerve medial brachialis
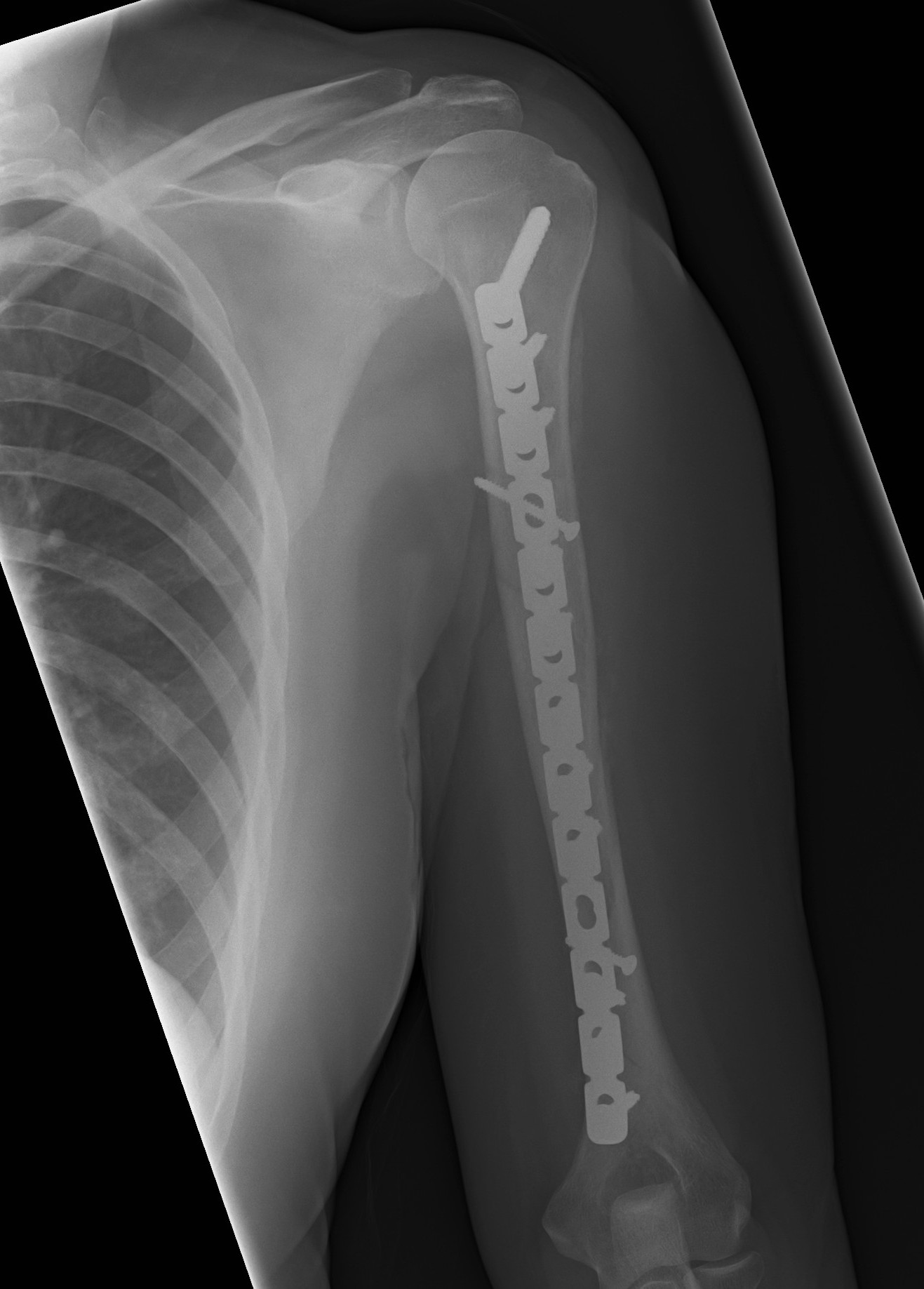
Plate
- narrow large fragment 4.5 mm DCP / long Philos proximal humeral plate
- minimum 6 cortices above and below
- can consider dual plate







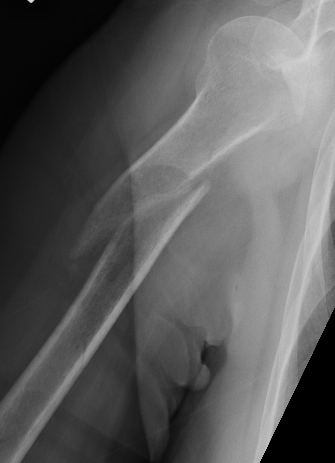
Failure of fixation
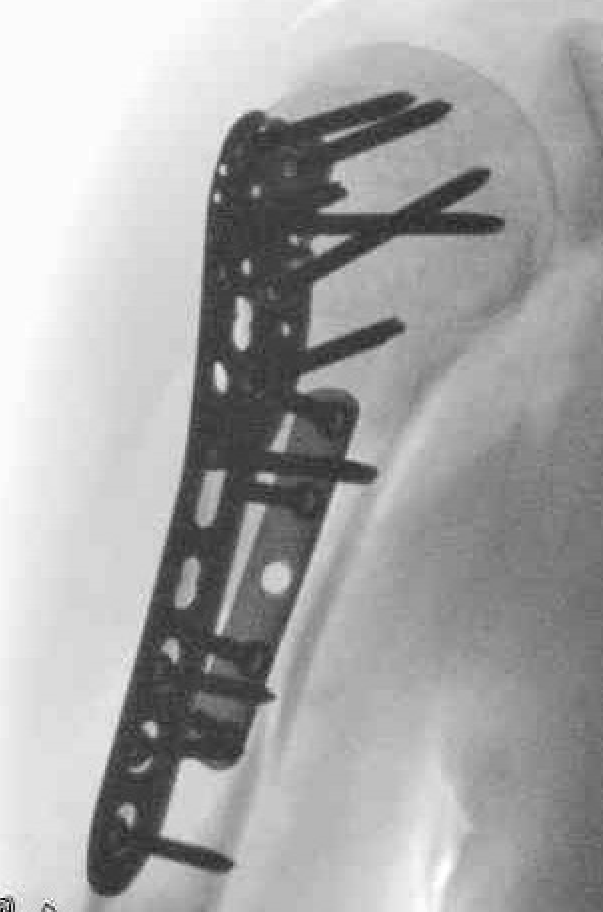
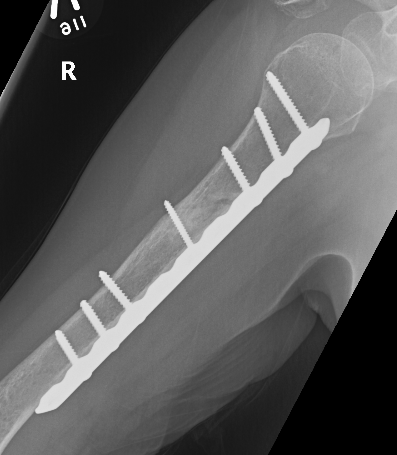
Minimally Invasive Plate Osteosynthesis (MIPO)
Concept
Bridge plating
Indirect fracture reduction
Indications
Surgical neck of humerus to 10 cm of elbow joint
Options
Anterior plating with narrow 4.5 mm LCP
Lateral plating with long proximal humerus plate
Jeong et al. BMC Musculoskeletal Disorders
- 18 patients treated with narrow LCP (anterior)
- 17 patients treated with long Philos plate (lateral)
- 2 metal failures in the Philos plate group requiring revision to LCP
Technique anterior MIPO plating

Position
- patient supine
- arm on arm table
- ensure can image proximal humerus
- keep elbow flexed to aid reduction and reduce biceps tension
Narrow LCP plate
- place on arm to select appropriate size



Incisions
Proximal 4 - 5 cm
- deltopectoral approach
Distal 4 - 5 cm
- anterior approach to distal humerus
- mobilise biceps laterally
- identify and protect lateral cutaneous nerve of the forearm
- split bracialis
- keep arm supinated to protect radial nerve
- avoid deep retractors laterally to protect radial nerve
Create submuscular plane
- periosteal elevator along bone
Precontour narrow LCP plate
- subtle convex curve proximally
- subtle concave curve distally
- 10 - 15 degrees internally rotated
Pass plate
- indirect fracture reduction
- secure plate proximally to bone
- reduce fracture
- distal fixation




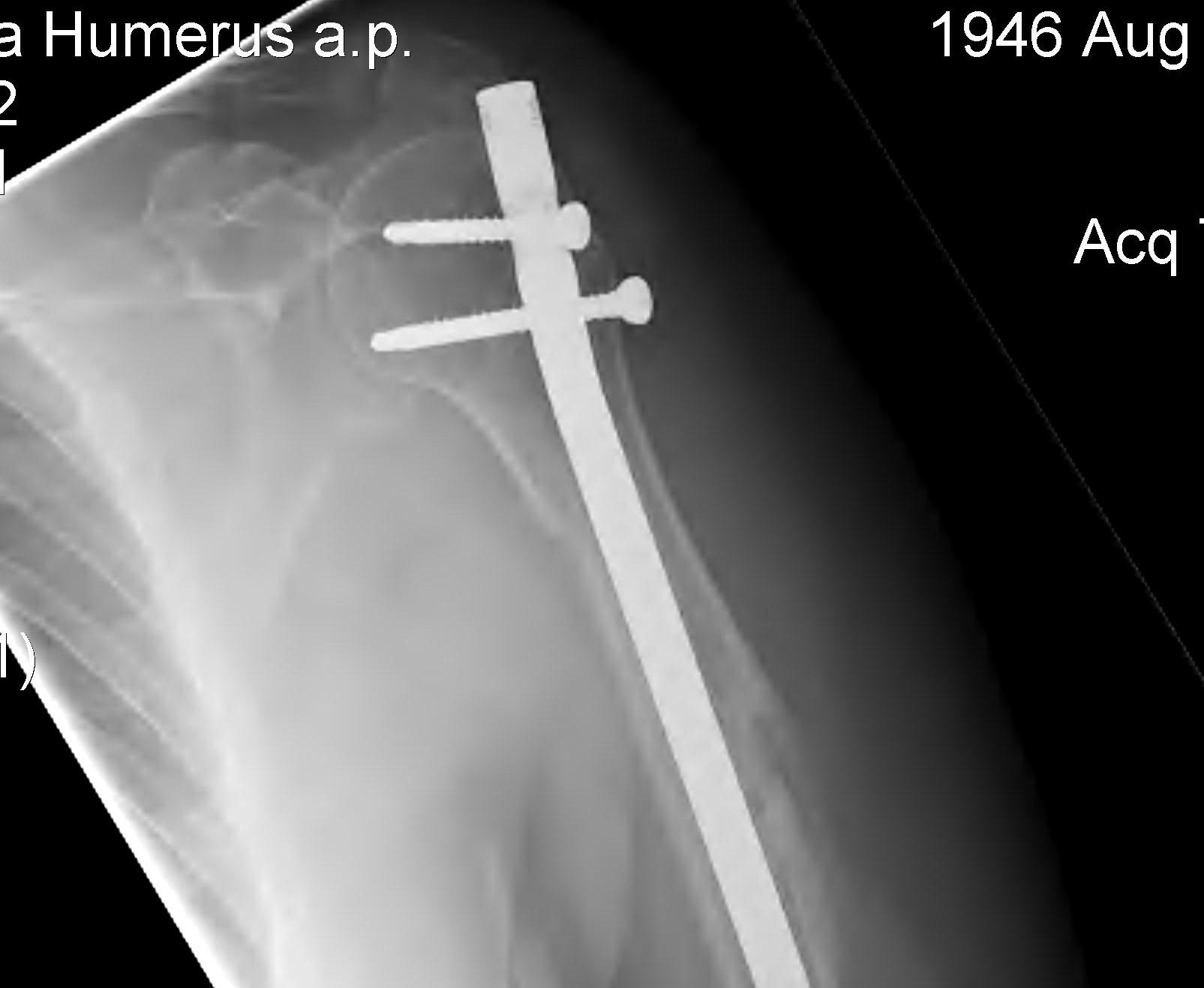
Antegrade Humeral Nail
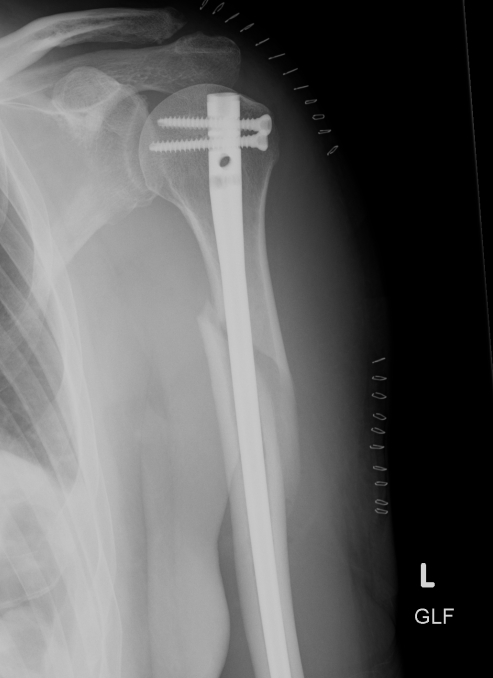
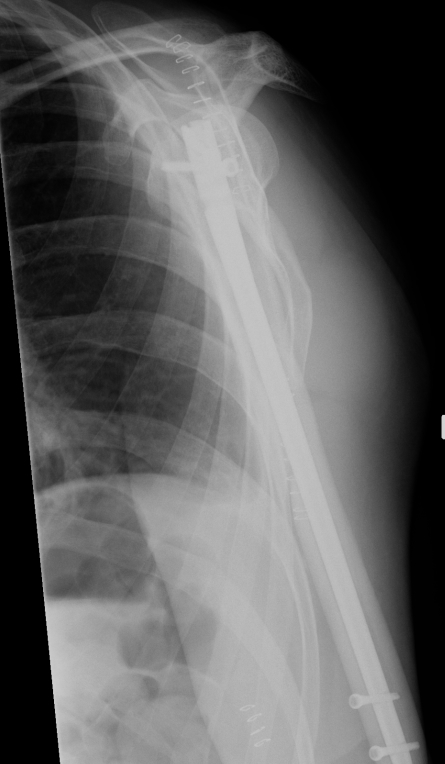
Relative indications
Segmental fracture - need very long plate
Impending pathological fracture
Obesity
Skin compromise
Technique
Set up
- lazy beach chair
- can do flat on bed, with bump under shoulder
- need to get fluoroscopy of shoulder and distal forearm
- have fluroscopy come from opposite side
- patient relatively supine to ensure ease of AP distal locking
Anterolateral approach shoulder
- longitudinal split supraspinatus
- can split at the anterior edge of supraspinatus, and retract posteriorly
- protect rotator cuff throughout
Entry with K wire or awl
- entry point at medial aspect greater tuberosity
- theorectically protects the cuff tendon
- check centred in humerus canal using fluoroscopy on AP and lateral
- increase diameter proximally with hand reamers
Pass guide wire
- can do closed
- can perform mini open incision over fracture site
- use finger to blunt dissect and protect radial nerve
Minimal reaming
Pass nail
- typically 7 mm
- ensure that nail is buried enough to protect cuff
- need to consider hardware removal
Proximal locking screws
- ensure not in joint
- lateral and anterolateral
- protect biceps tendon
Distal AP locking screw/s
Careful repair of rotator cuff
Complications
Rotator cuff pain
- must not leave nail prominent
- must carefully repair cuff
Management Nonunion Humerus Fractures
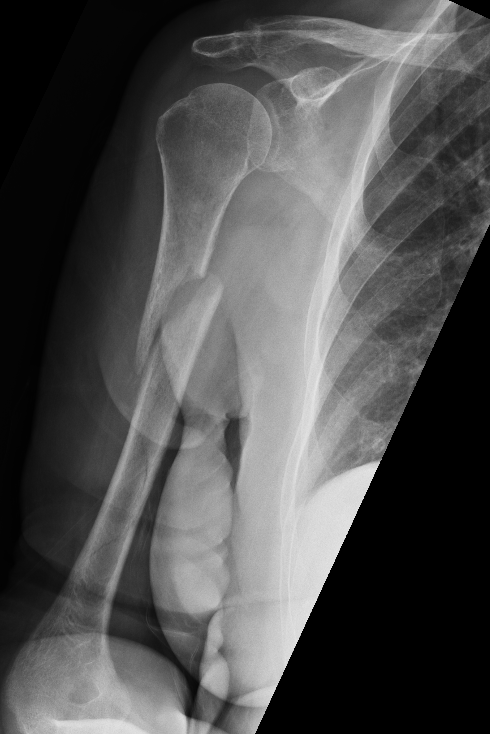
Background
Definition
Mean time to union is 13 weeks
No evidence of callous on xrays taken 6 - 8 weeks apart
Fracture patterns
- highest risk is transverse fractures
- proximal humerus shaft fractures also at risk due to displacing force of pectoralis and deltoid, and LHB may interpose
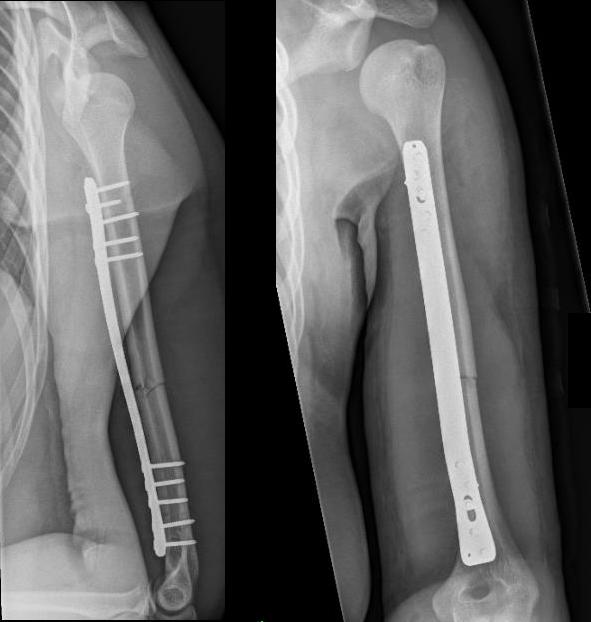
Management
- systematic review of union rate after operative intervention of humeral shaft non union
- plate only 95%
- plate and bone graft 98%
- IMN 66%
- IMN + bone graft 88%
- external fixation 98%
Technique
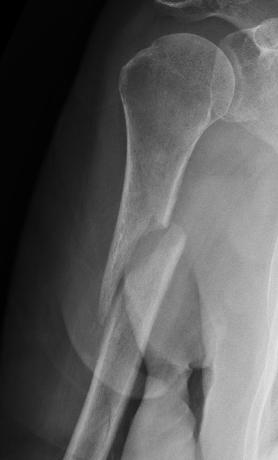
Approach
- fracture site dependent
- 4.5 mm plate with 6 cortices above and below
- if use 3.5 mm long proximal humeral plate, suggest 8 cortices below
- use iliac crest bone graft
- consider dual plating in proximal fractures with insufficient fixation, or in poor bone quality
Complications of ORIF
Nonunion
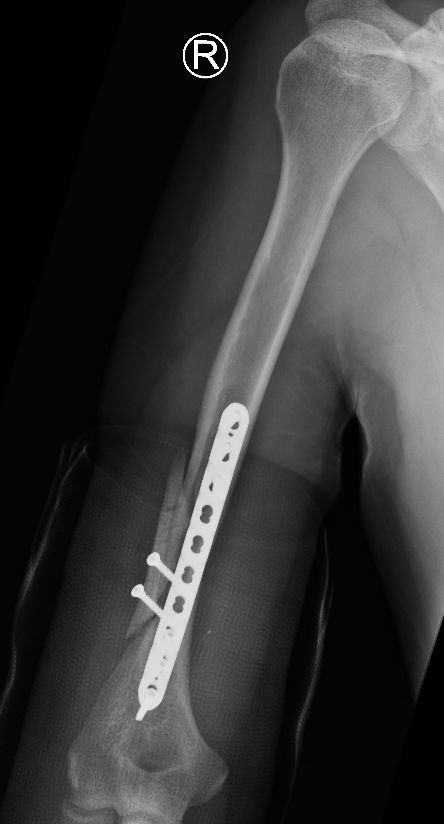



Revision of fixation to longer posterior plate
Infection


