Complications
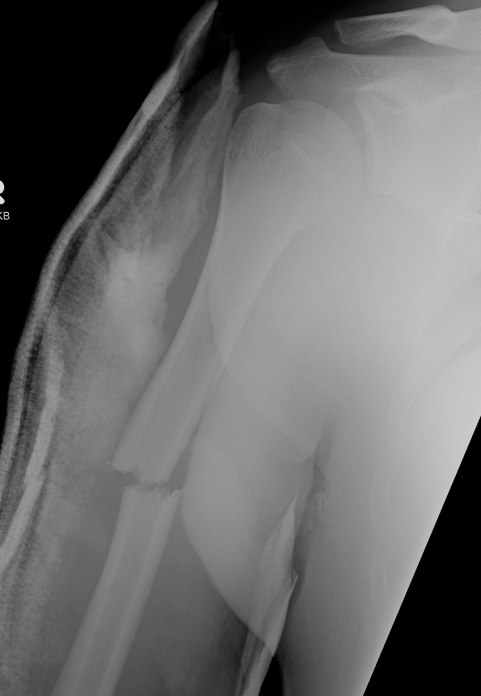
Intraoperative glenoid fracture
Avoid by
- careful reaming and drilling osteoporotic bone
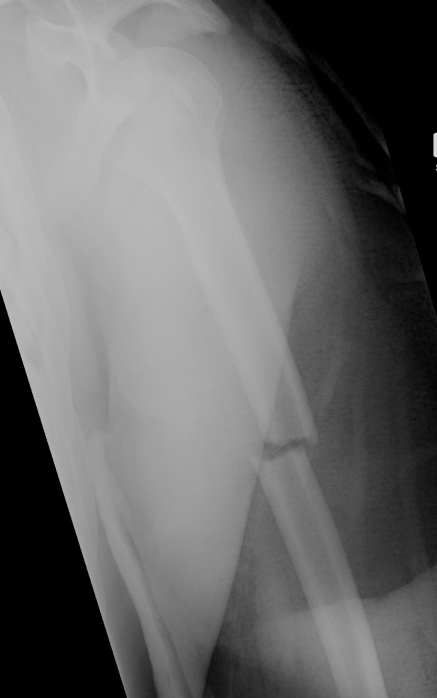
Management
1. Rotate metaglene
- use locking screws to stabilise glenoid
2. PA screws
- cannulated 4.0 mm screws
- inserted percutaneously from posterior
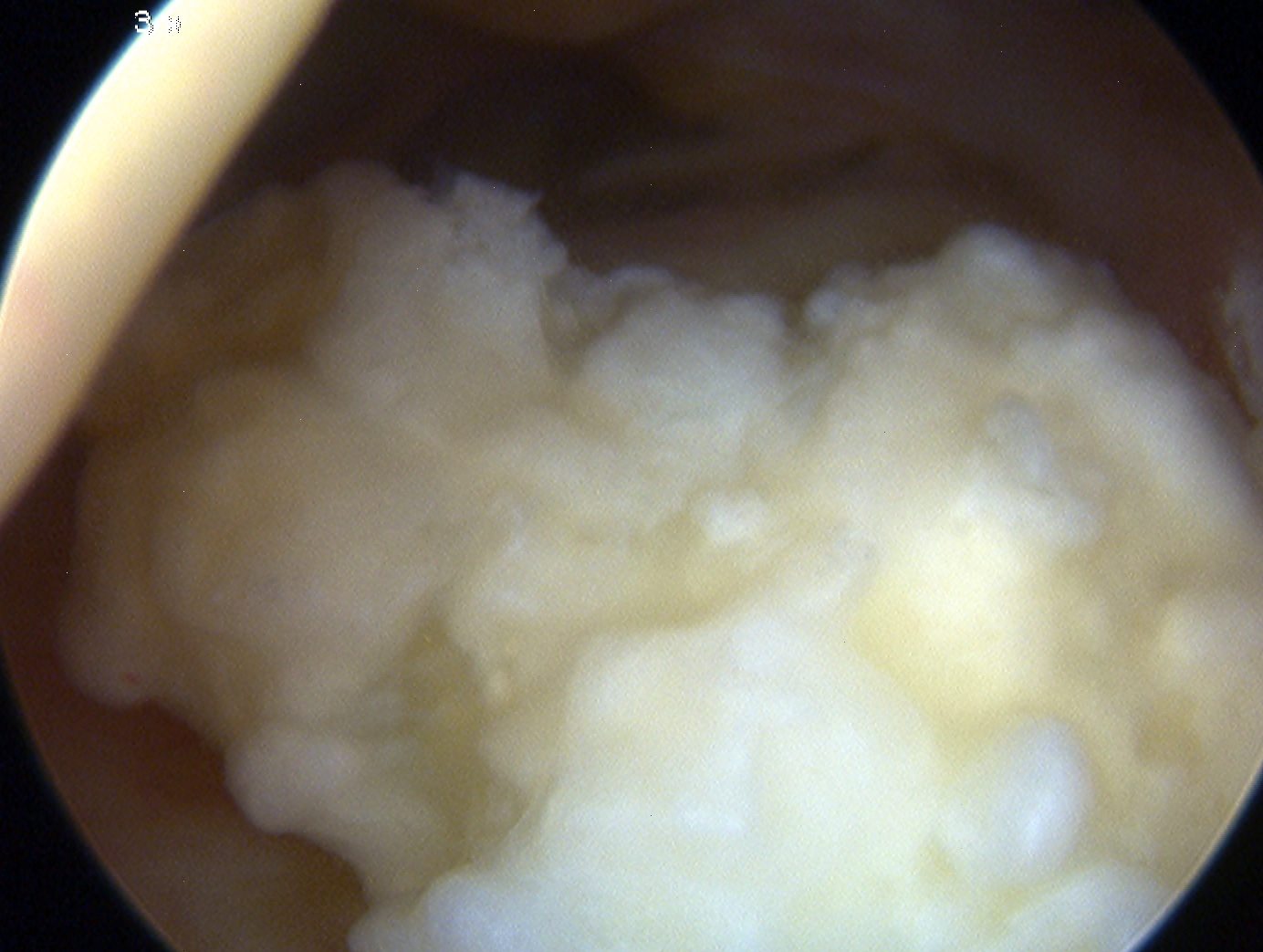
Haematomas
Great deal of dead space is created
- always use a drain