Selection of Level
Aim to preserve foot if possible
Biologic Amputation Level
- most distal functional amputation level
- with reasonable potential for wound healing
Levels
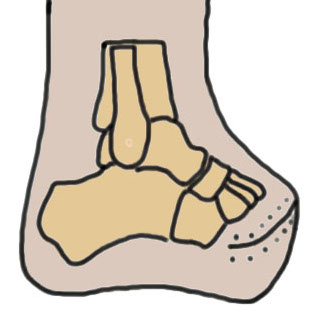
Forefoot - toe / ray / transmetatarsal
Midfoot - Lisfranc / Chopart
Hindfoot - Boyd / Pirogoff / Syme
Transtibial - below knee amputation
Forefoot amputations
Toe amputations

Technique
- dorsal-plantar or side-to-side flaps
- fish mouth
Great toe
- never through MTPJ due to increased plantar pressure
- either base proximal phalanx or proximal to metatarsal neck
- must stabilise sesamoids or they retract & expose base metatarsal
Lesser toes
- avoid 2nd toe amputation because of risk of severe hallux valgus
- if removing multiple toes never leave a single toe
- consider transmetatarsal amputation in this setting
Results
Viquez-Molina et al Int J Low Ext Wounds 2025
- 185 diabetics undergoing toe amputation
- up to 1/3 failed and required more proximal surgery
Ray amputation

Definition
Remove a single metatarsal and toe
Technique
Medial ray - can remove single ray only
Lateral ray - can remove up to two
Central ray - may be inferior to Lisfranc amputation
Results
Haller et al J Foot Ankle Surg 2020
- ray resection in 185 patients
- 38% revision rate (27% minor amputation, 11% major amputation)
Transmetatarsal amputation
Technique
- longer plantar flap
- preserve tibialis anterior and peroneus brevis attachments
- preserve metatarsal cascade
- avoid sharp edges
Midfoot amputations
van der Wal et al Medicine 2023
- systematic review of Lisfranc v Chopart amputation
- Lisfranc: failed wound healing 20%, ambulation 85%
- Chopart: failed wound healing 28%, ambulation 74%
Lisfranc Amputation
Tarsometatarsal amputation
Technique
- long plantar flap
- preserve insertion of tibialis anterior and peroneus longus
- preserve base of 5th metatarsal / insertion peroneus brevis
- prevents supination
- +/- tendo achilles lengthening
- leave cartilage surfaces if not infected
Chopart Amputation

Midtarsal amputation
Modified Chopart: tendon balancing
Technique
- preserve talus and calcaneus
- avoid equinus and varus
- fish mouth incision
- divide talonavicular and calcaneocuboid joint
- Z lengthen achilles tendon
- reattach tibialis anterior to neck of talus
- reattach tibialis posterior to talus
- reattach peroneus brevis to calcaneus
Results
- 18 Chopart amputations in diabetes
- 94% developed postop wound complications
- only 44% successfully ambulated with prosthesis
- 55% revision to Syme / BKA
Fagilia et al J Foot Ankle Surg 2016
- 83 Chopart amputation in diabetes
- 56% healed
- 28% required further amputation
- 25% annual death incidence
Hindfoot Amputation
Issues
Uncommon in diabetes
1. Limited surface area remaining
- high risk of ulcer
2. Must have good posterior tibial artery perfusion
3. Often associated with leg length discrepancy and risk of falls
4. More complicated prostheses
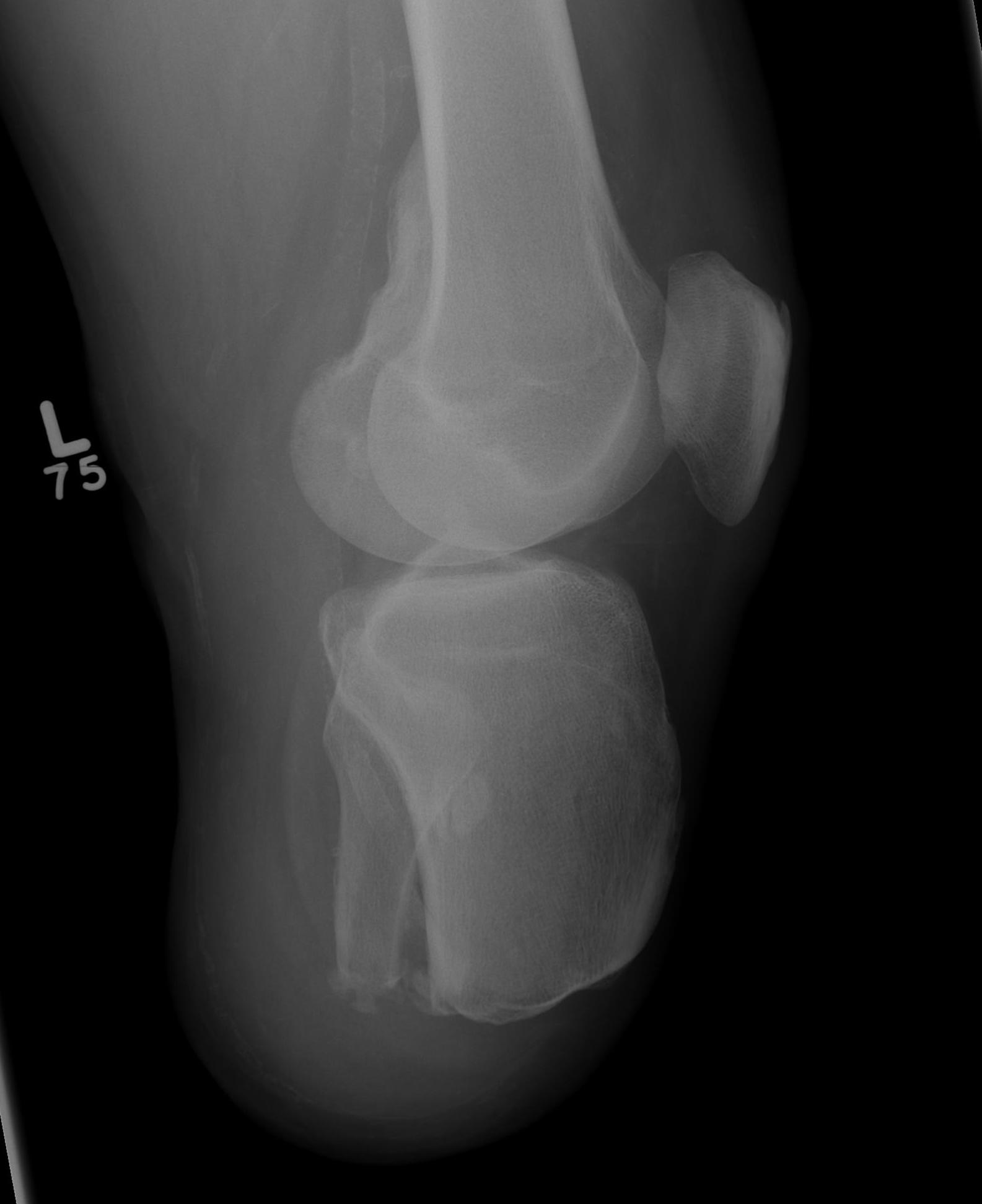
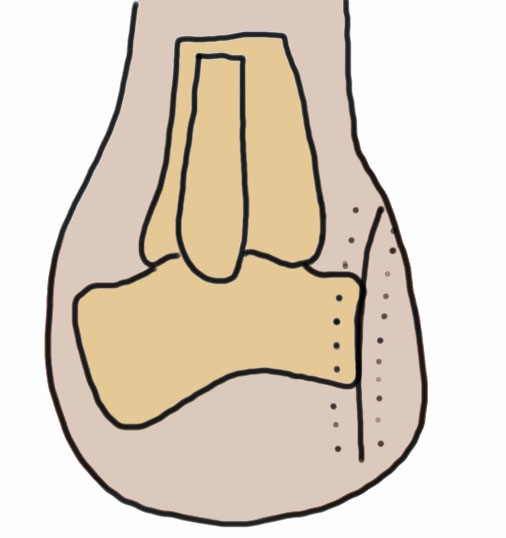
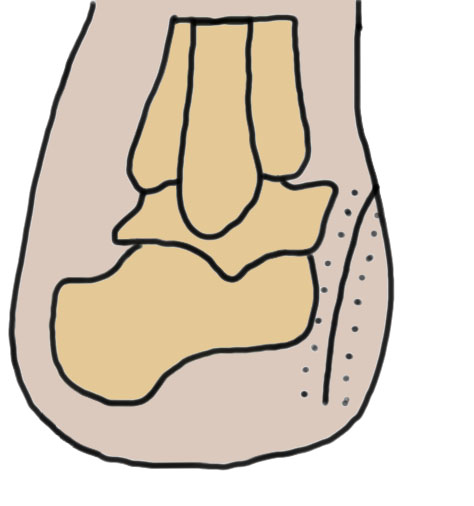
Boyd / Pirogoff amputation
Concept
- Boyd: talectomy and calcaneotibial arthrodesis
- Pirogoff: talectomy and calcaneotibial arthrodesis with partial calcaneal resection
- forward translation of the calcaneus
- fixation to obtain fusion
Technique
- dorsal incision from tip lateral malleolus to medial malleolus
- planter incision transversely across sole at level metatarsal bases
- amputate forefoot through Chopart joint
- excise talus
- anterior calcaneal osteotomy transversely across calcaneum at level of peroneal tubercle
- shift calcaneum anteriorly
- excise cartilage of distal tibia / fibula & superior calcaneum
- calcaneo / tibial arthrodesis
Issues
- prolonged non weight bearing periods to obtain fusion
- small surface area / risk of ulcers
- risk of nonunion of arthrodesis
- LLD of 2 - 4 cm
- need custom AFO to ambulate
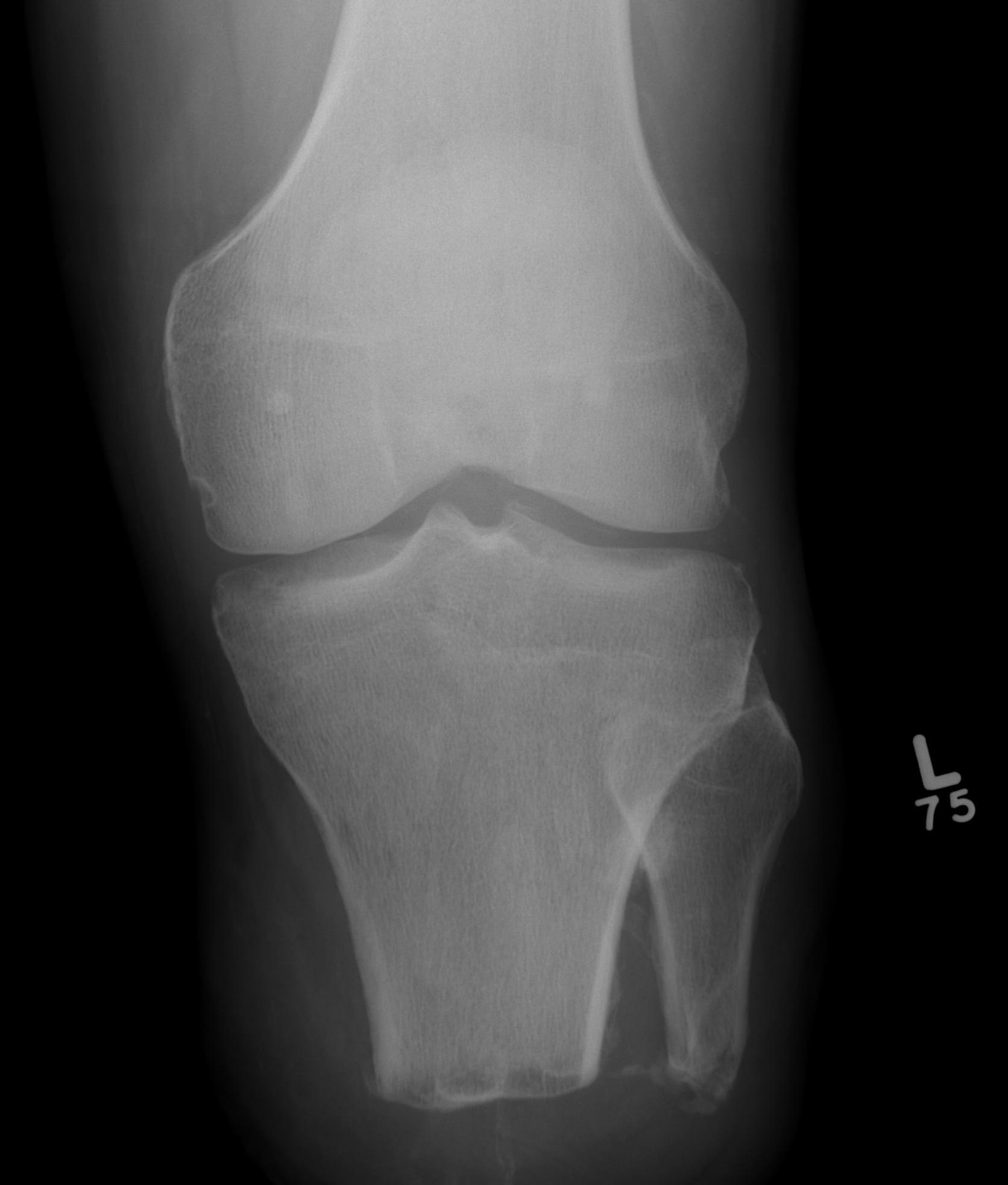
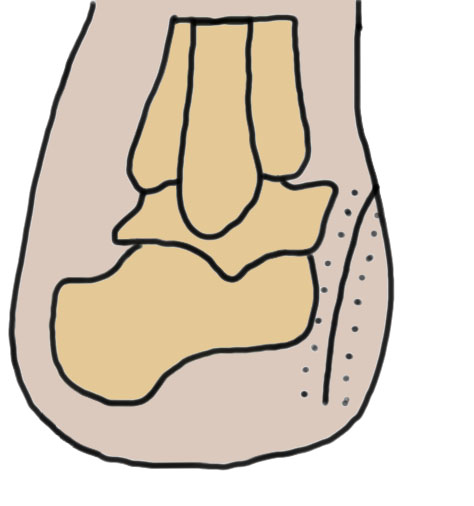
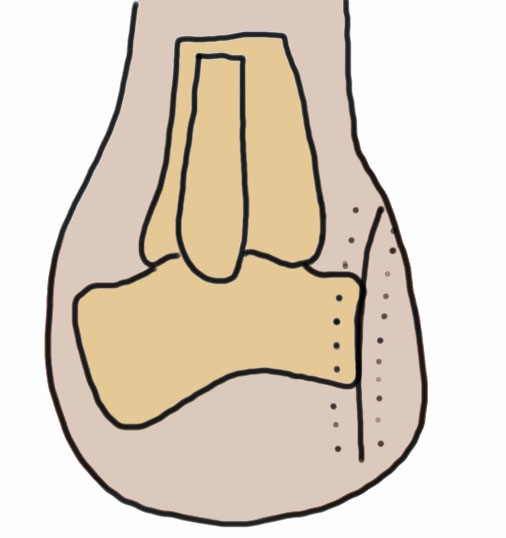
Syme's amputation
Concept
- ankle disarticulation
- remove talus and calcaneum
- remove both malleoli
- preserve heel pad
Technique
- incision from tip of lateral malleolus to medial malleolus across front of ankle
- then continue plantar under sole between same points / MT bases
- need to preserve large post heel pad
- excise talus & calcaneus
- remove malleoli at level of joint & contour
- divide arteries / veins / nerves above levels of flaps
- anchor heel pad to anterior tibia via intra-osseous sutures
Issues
- small surface area / risk of ulcers
- LLD of 4 - 7 cm
- custom AFO
Trans-tibial amputation
www.boneschool.com/amputations-about-the-knee
Technique
Long posterior flap
- keep long tibial stump
- fibular cut 1 - 2 cm shorter
- gastrocnemius myodesis