nonunion
Distal Tibial Fractures
Distal Tibial Fractures
Definition
Metaphyseal
Extra-articular
Intra-articular Extension
ORIF displaced in young
Indications
< 60 with good bone stock and preserved joint space
Reduction
Union rates increased with anatomical reduction
Options
- closed reduction
- open reduction / if closed reduction fails
Accept
- no varus
- < 15o valgus
- < 10o AP plane
Non Union
Definition
Non-union
- arrest of progression to union at fracture site
- > 6-9 /12
- no visible progressive signs of healing for at least three consecutive months
- individualise for each fracture
- when the surgeon believes the fracture has little or no chance to heal
Delayed union
- failure of fracture to unite within expected time
- still may spontaneously unite
Patella Fracture
Mechanism
Direct blow
- most common
Indirect
- forced knee flexion with foot fixed / maximally contracted quadriceps
Types
1. Vertical

2. Transverse
Femoral Shaft Fractures
Epidemiology
Usually young patients
- 15 - 40
15% compound
Aetiology
High velocity injury
- MBA
- MVA
- pedestrian v car
- fall from height
Emergency Managment
EMST principles
- need for transfusion not uncommon
Management
Acute management
Resuscitation
EMST
Neurovascular assessment
Investigations - exclude Pipkin, NOF
Emergent reduction / skeletal stabilisation
Assess stability
Re-evaluate sciatic nerve
Insertion Femoral Steinman Pin
Indications
- displaced acetabular fracture
Midshaft Tibial Fracture
Epidemiology

Most common long bone fracture
Aetiology
Young patients / sports
Elderly / simple falls
MVA - often compound
Tscherne Soft Tissue Classification
Grade 0
- nil ST injury
Grade 1
Intertrochanteric Fractures
Definition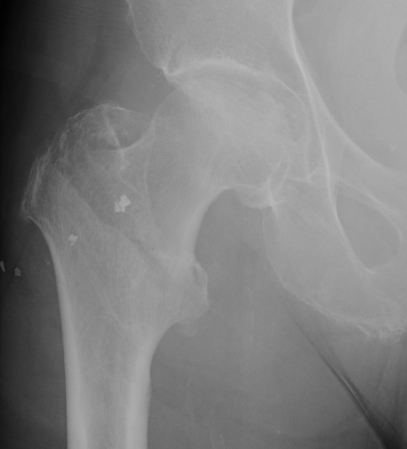
Fracture which extends between the trochanters of the proximal femur
- lower limit is inferior border of lesser tuberosity
Anatomy
Extra capsular / well vascularized
The key to stability is the posteromedial cortex

