


Indications
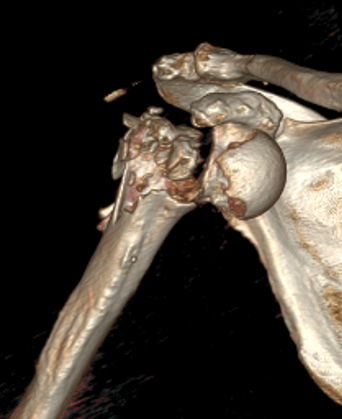
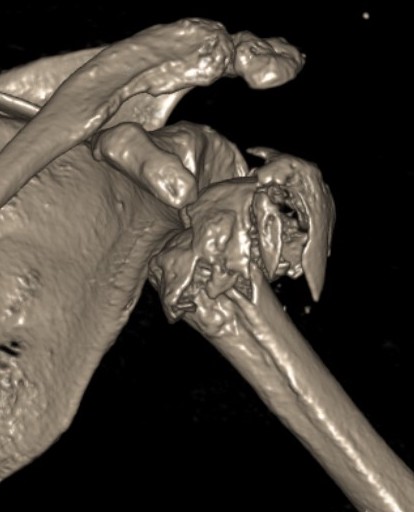
Severe comminuted proximal humerus fractures
100% displaced / off ended
Fracture - dislocations


Arthroplasty options
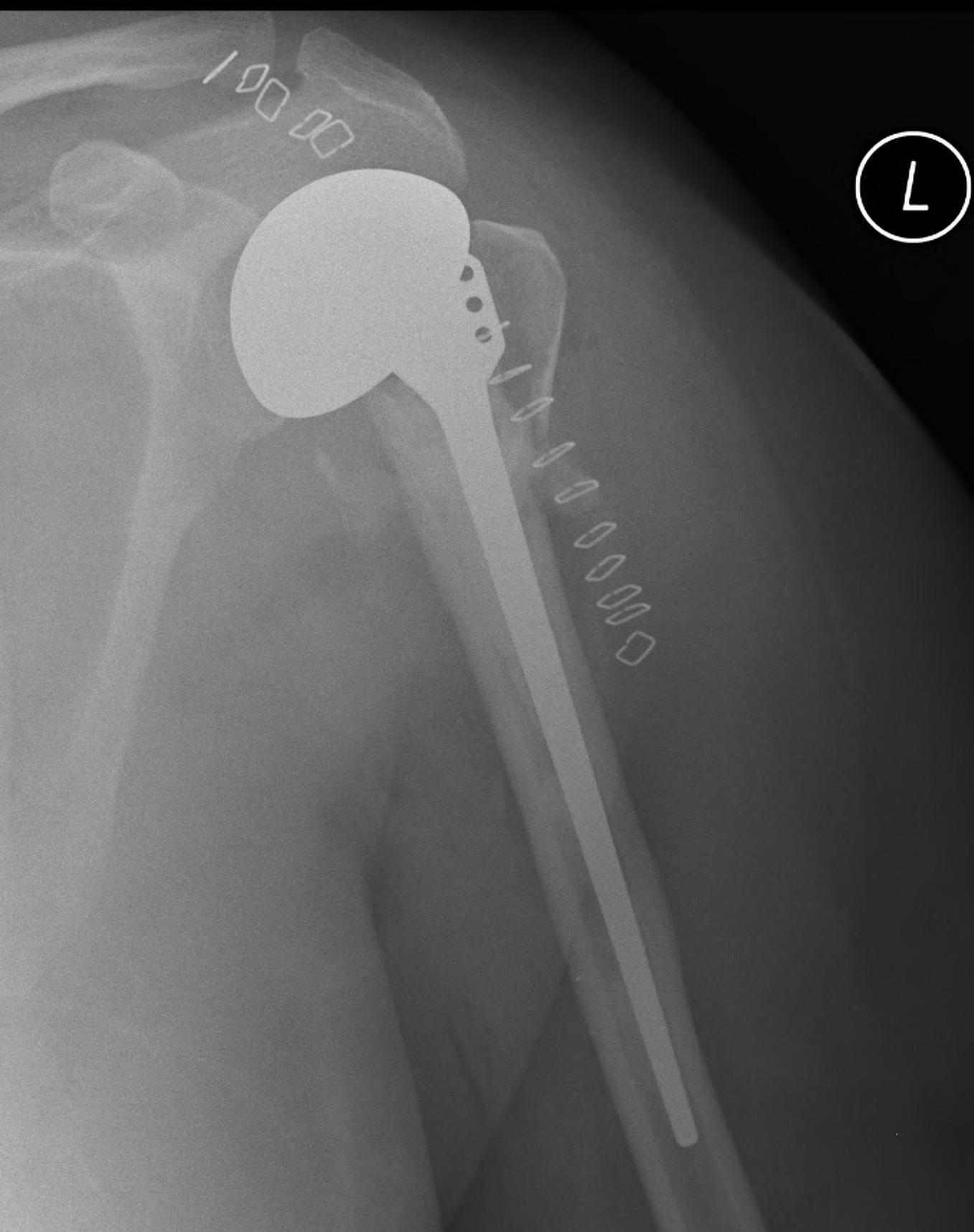
Reverse total shoulder arthroplasty
- elderly patients
- better outcomes than hemiarthroplasty
Hemiarthroplasty
- young patients with unreconstructable fractures
- too young for rTSA
Reverse TSA versus hemiarthroplasty
- RCT of 99 patients rTSA v hemiarthroplasty
- > 70 years and displaced 3 or 4 part SNOH fracture
- 10 point better Constant score with rTSA
- better ROM with rTSA: abduction 110 v 80, flexion 125 v 90
Austin et al J Orthop Trauma 2019
- systematic review of hemiarthroplasty v rTSA
- > 65 with SNOH fracture
- 15 studies and 900 patients
- rTSA better pain scores, functional outcome, ROM and lower reoperation rates
Reverse total shoulder arthroplasty
Indications
Unreconstructable fracture in elderly > 65
- comminuted, 3 or 4 part
- head spltting fracture
- off ended / 100% displaced

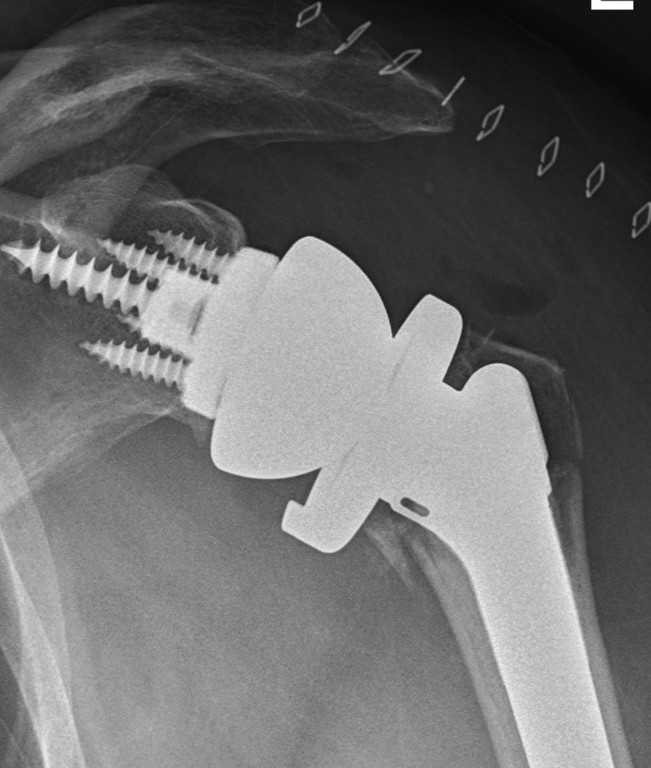



Technique
Vumedi reverse TSA for fracture video
www.boneschool.com/rTSA-technique
Results
rTSA for proximal humerus fracture versus rotator cuff arthropathy
- systematic review of rTSA for proximal humerus fracture v rotator cuff arthropathy
- worse clinical outcomes and ROM for fracture treatment
Revision rate
Australian Joint Registry 2024
| Indication | 1 year | 5 year | 10 year | 14 years |
|---|---|---|---|---|
| Rotator cuff arthropathy (n=20,500) | 2.3 | 4.2 | 5.4 | 6.1 |
| Osteoarthritis (n=24,000) | 1.9 | 3.5 | 5.0 | 6.7 |
| Fracture (n=8,000) | 3.1 | 4.8 | 5.9 | 5.9 |
Cemented versus uncemented
Kao et al Eur J Orthop Traumatol 2023
- systematic review of 34 studies cemented v uncemented rTSA for proximal humerus #
- improved Constant score with cemented rTSA
- no difference in complications
- systematic review of 45 studies cemented v uncemented rTSA for proximal humerus #
- no difference in outcomes
- high complication rate uncemented rTSA 10% v cemented 6%
Tuberosity fixation / healing
- rTSA for proximal humerus #
- improved functional outcomes with tuberosity healing
- systematic review of 800 patients with rTSA for fracture
- improved forward flexion and abduction with tuberosity healing
Complications
- systematic review of complications after rTSA for fracture
- 100 studies and 10,000 cases
- overall complication 7%
- instability 2%
- infection 1%
- periprosthetic fracture 1%
- revision rate 3%
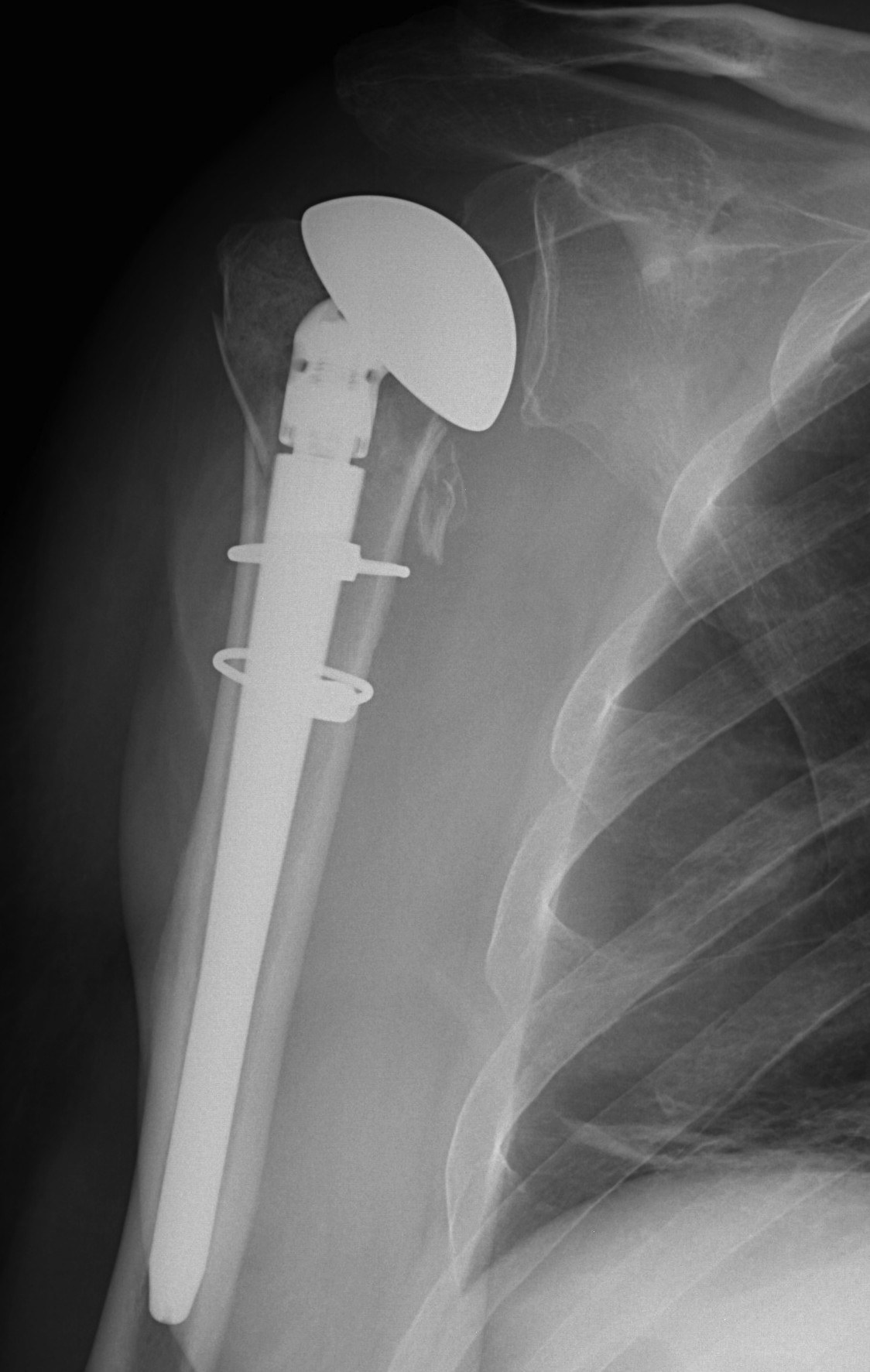
Hemiarthroplasty
Indications
Unreconstructable fracture - 4 part, comminuted, head spltting fracture
Insufficient glenoid
Patients too young for rTSA



Technique
Beach chair / deltopectoral approach
- need to be able to extend humerus to insert stem
Extensile approach
- release CA ligament
- release proximal pectoralis major
- release anterior deltoid insertion from lateral clavicle if needed (intra-osseous repair later)
- protect musculocutaneous nerve under conjoint, minimal retraction
- protect the axillary nerve on inferior border of SSC medially
Tuberosities
- identify and release biceps tendon
- identify and tag greater and lessor tuberosities with Mason Allen sutures
Prosthesis
Remove and size anatomical neck
- identify diameter and thickness
- ream humerus and trial stem
Humeral height
- trial with arm hanging to replicate weight
- will usually need to leave stem proud from fracture
- should be able to anatomically restore tuberosities
- cement stem with retroversion of 30o
Repair tuberosities to the humeral stem
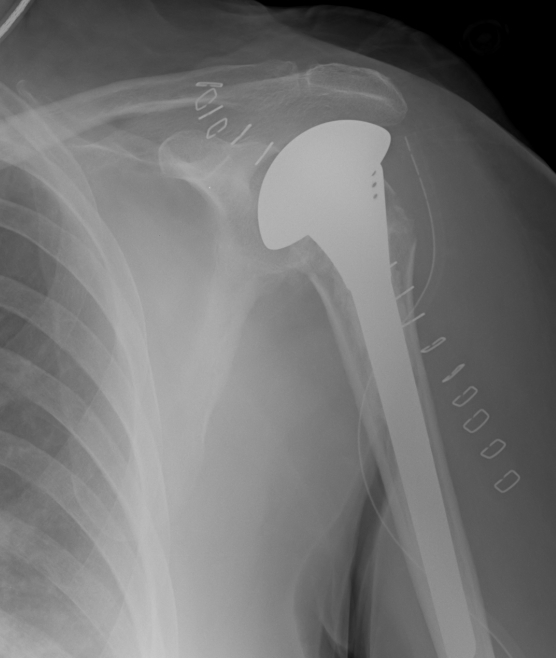
Results
- 14 year outcome of 87 HA for proximal humerus fractures
- 10 year survival 97%
- mean Constant score 80
- mean forward flexion 125 degrees
- 22% greater tuberosity complications - worse outcomes
- 65% glenoid wear - worse outcomes
Complications

Loss of tuberosity fixation
