

Definition
Fracture of the radial shaft with disruption to the distal radio-ulna joint (DRUJ)
Fracture-dislocation
Incidence
DRUJ instability
- usually dorsal instability
- volar instability rare
Anatomy
Supination / pronation
- rotation of the radius around the ulna
- contribution of the radial bow (average 15 mm)
| Proximal radio-ulna joint | Distal radio-ulna joint | Inter-osseous membrance |
|---|---|---|
|
Radial head & lesser sigmoid notch ulna |
Ulna head & lesser sigmoid notch radius | Longitudinal forearm stabilty |
| Annular ligament |
TFCC Dorsal / volar radioulnar ligaments |
Central band most important |
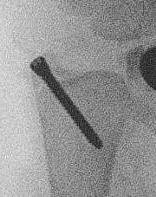
Xray
DRUJ disruption
- widened space between radius and ulna on AP
- dorsal subluxation / dislocation of ulna on lateral
- radial shortening > 5 mm
- ulna styloid fracture
Shortening of radius with disruption of DRUJ on lateral


Widening of interval between radius and ulna / clear disruption of DRUJ


Concern for disruption of DRUJ on lateral
Operative management
Algorithm
1. Anatomical ORIF of distal radius with dynamic compression plate
- anatomical reduction
- restoration of radial bow
- compression for healing
2. Assess DRUJ stability
- if stable in supination can cast in supination
Radius ORIF with dynamic compression plates


Sukpanichyingyong et al J Clin Orthop Trauma 2023
- RCT of 54 stable Galeazzi fractures
- 2 versus 4 weeks immobilization
- no difference in functional outcome
DRUJ instability after radius ORIF
Related to location of radial fracture / more likely with fracture < 7.5 cm to articular surface
Rettig et al J Hand Surg Am 2001
- 40 patients with Galeazzi fracture dislocations
- DRUJ instability after radius ORIF
- Type 1: radius fracture < 7.5 cm to articular surface: 55% DRUJ instability
- TYpe II: radius fracture > 7.5 cm to articular surface: 6% DRUJ instability
Korompilias et al J Hand Surg Am 2011
- 95 patients with Galeazzi fracture dislocations
- 69 Type I distal third: 54%
- 17 Type II middle third: 12%
- 9 Type III proximal third: 11%
Options
| K wire stabilization | ORIF ulna styloid fracture | Repair TFCC |
|---|---|---|
|
2 x 1.6 mm K wires Proximal to sigmoid notch Ulna to radius Ensure K wire exits radius in case of breakage |
Hook plates K wire and TBW |
5/6 approach - bed of EDM - interval between EDM and ECU - open capsule - repair TFCC |
 |
 |
 |
| AO surgery K wire fixation DRUJ |
AO surgery ulna styloid fracture screw fixation AO surgery ulna styloid TBW fixation
|
|
Results
Some evidence that K wire stabilization better than TFCC repair
- systematic review of 258 cases of DRUJ instability after radius ORIF
- cast in supination v TFCC repair v K wire DRUJ
- persistent DRUJ instability 1% with no between group differences
- reduced grip strength and ROM with TFCC repair


Irreducible DRUJ dislocations
Can be soft tissue blockage / usually extensor tendons
- systematic review of 17 cases of irreducible Galeazzi fracture-dislocations
- 90% blocked by extensor tendon
- remainder blocked by fracture fragment
- 7/66 (11%) incidence of DRUJ instability after fixation
- 4/7 had ulnar styloid fracture
- may need ORIF ulnar styloid / fixation of TFCC to obtain stability
- can pin DRUJ proximal to fossa


