

Anatomy
Supination / pronation
- rotation of the radius around the ulna
- contribution of the radial bow (average 15 mm)
| Proximal radio-ulna joint | Distal radio-ulna joint | Inter-osseous membrance |
|---|---|---|
|
Radial head & lesser sigmoid notch ulna |
Ulna head & lesser sigmoid notch radius | Longitudinal forearm stabilty |
| Annular ligament |
TFCC Dorsal / volar radioulnar ligaments |
Central band most important |
Compartment syndrome
Incidence
Auld et al J Orthop Trauma 2017
- 151 BBFF
- 15% underwent fasciotomy
- increased risk with high energy / highly comminuted / segmental fractures
Management
AO surgery reference forearm compartment syndrome
Release all 3 compartments in forearm (mobile wad / volar / dorsal)
- Henry approach - release mobile wad / deep and superficial flexor compartments / carpal tunnel
- Dorsal approach to ulna - release ECU
Compound wounds
Nonoperative management
Indications
Extremely uncommon
- adult BBFF very unstable fractures
- malunion results in loss of supination / pronation




Radial fracture malunion requiring corrective osteotomy
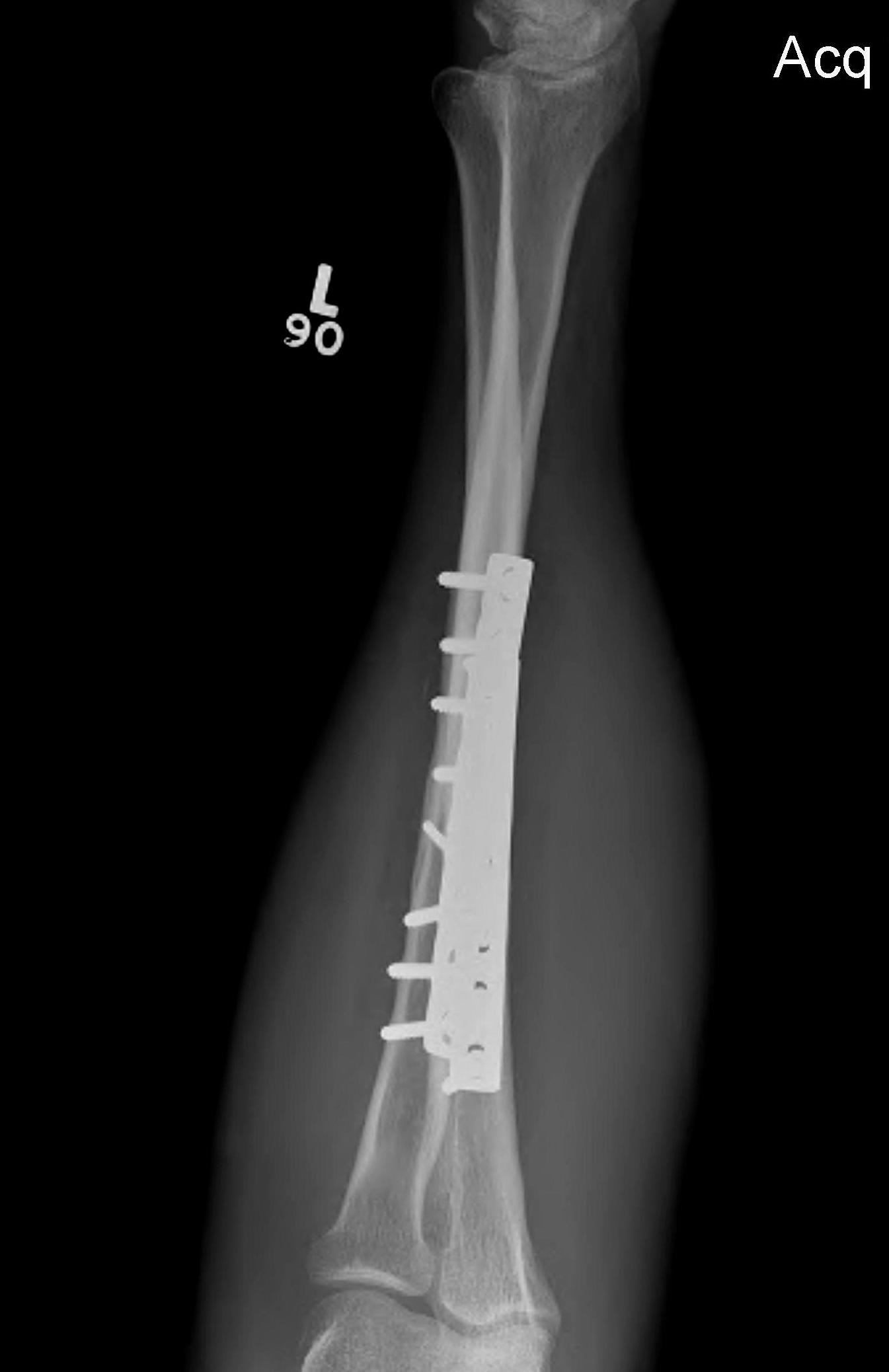
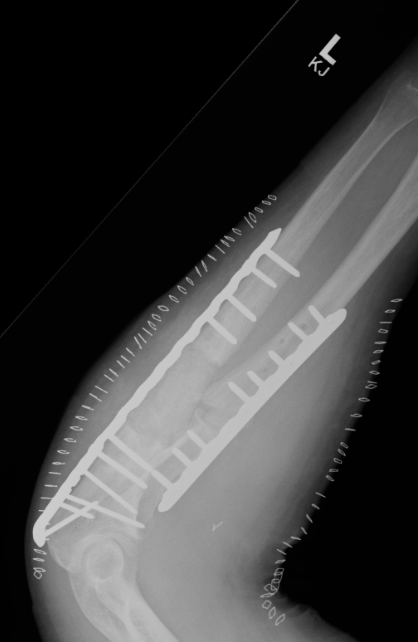
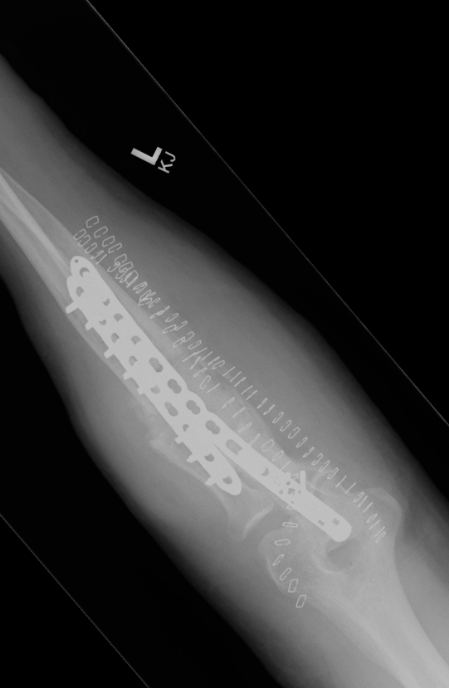
Operative management


Options
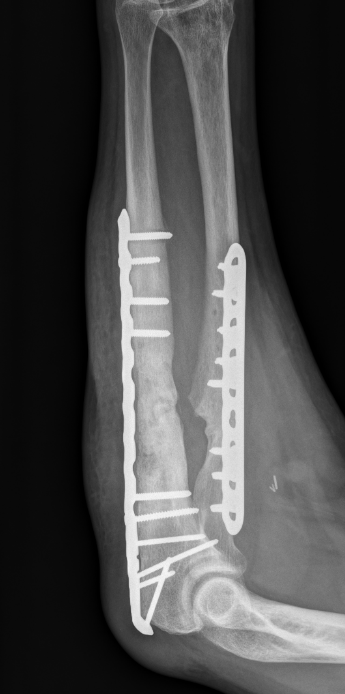
ORIF with plates
Intramedullary fixation
Results
Outcomes
- 30 BBFF fractures followed for 5 years
- supination / pronation 90%
- strength 70%
Plate versus IMN
Box et al J Orthop Surg Res 2024
- systematic review
- 9 studies comparing IM nail v plate fixation in adults
- no difference in outcomes or union rates
Lari et al J Orthop Traumatol 2024
- systematic review
- similar outcome scores with IMN and plate fixation in adults
- shorter operative times with IMN
- 11 cases of EPL rupture with IMN
Locking versus dynamic compression plates
Tseng et al J Orthop Traumatol 2025
- 500 patients with forearm fractures
- nonunion locking plates: 19%
- nonunion locking compression plates: 11%
- nonunion dynamic compression plates: 6%
ORIF with DCP plates
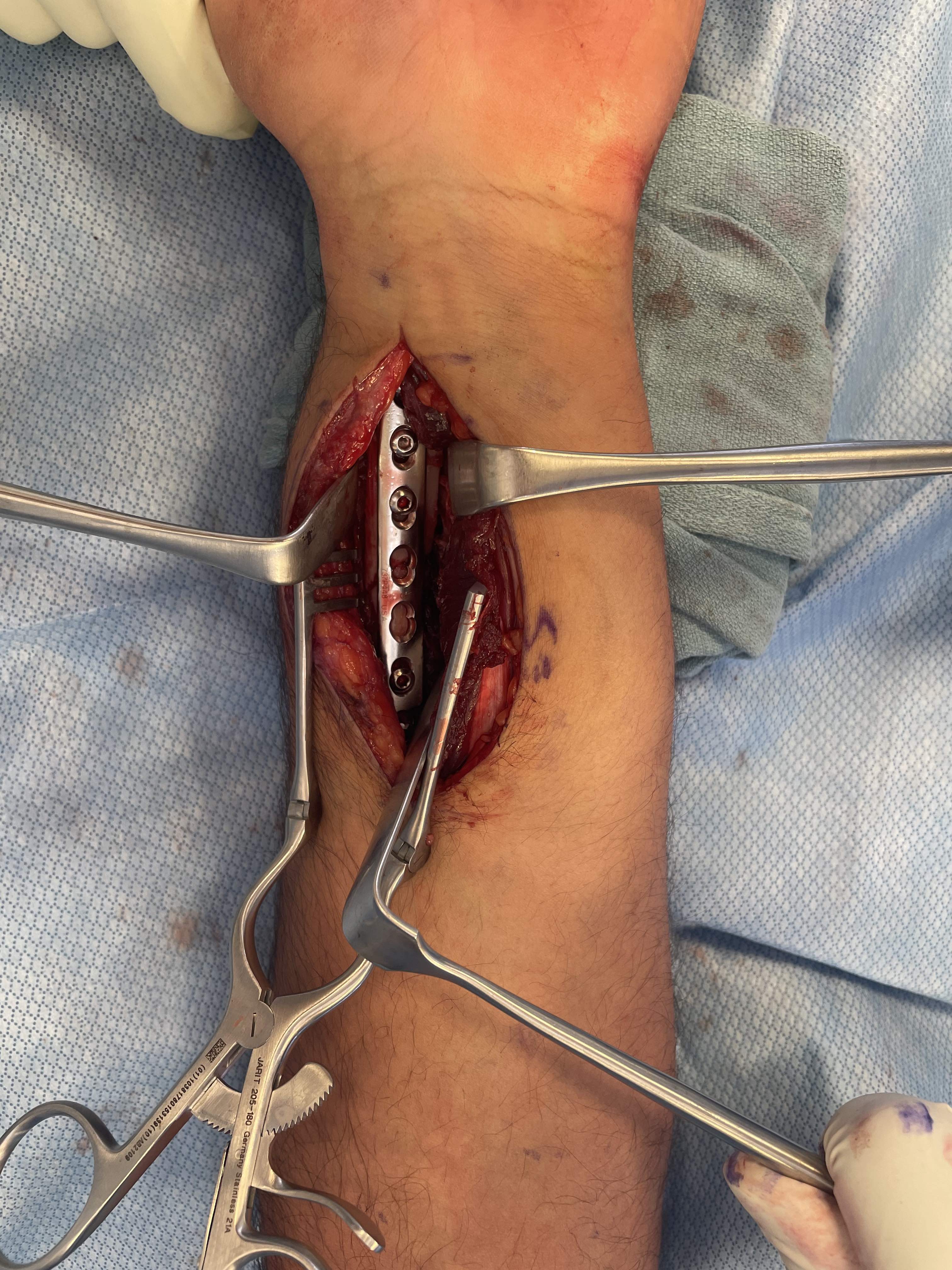


Approach
Radius - anterior Henry approach to radius
AO surgery reference anterior approach to radius
Proximal 1/3
- between mobile wad / bradioradialis and FCR
- ligate radial recurrent vessels and mobilize radial artery medially
- supinate forearm
- elevate supinator from ulna to radial
Middle 1/3
- between mobile wad / bradioradialis and FCR
- protect radial artery and venae comitantes
- detach pronator teres tendon from radial shaft as necessary
Distal 1/3
- between FCR and radial artery
- detach pronator quadratus
Ulna - approach between ECU / FCU
AO surgery reference approach to ulna
Protect dorsal branch of the ulna nerve distally
Fixation with DCP plates




Complications
Nonunion



Incidence
5%
Most common midshaft - reduced blood supply and maximal pronation / supination
Related to
- open fractures
- infection
- poor initial fixation / lack of compression
Type
Hypertrophic - adequate biology, unstable
Atrophic - inadequate biology
Investigation
Exclude infection: WCC > 11, ESR > 30, CRP > 2
Vit D
TSH / PTH
Alk Phos
Options
Revision compression plating + drill intra-medullary canals + autograft
Results
- 35 forearm nonunions treated with revision compression plating and bone grafting
- average defect 2 cm
- 100% union
Infected nonunion
Options
Masquelet induced membrane technique - defects up to 5 cm
Vascularized fibular bone graft - defects > 5 cm
Masquelet
- 32 infected forearm nonunions
- first stage: removal hardware / antibiotic cement for 6 weeks
- second stage: cancellous bone graft + plate
- 100% union rate





Malunion
More common with nonoperative management of pediatric forearm fractures
- loss of ROM
- failure to restore radial bow
www.boneschool.com/pediatric-forearm-fractures
Radio-ulna synostosis
Definition
Fusion between radial and ulna that limits rotation
Risk factors
High energy injury / comminution / open fractures
BBFF at same level / Monteggia
Traumatic brain injury
Delay in surgical treatment
Management
Excision
- wait for maturation between 1 and 2 years
- resection of synostosis
- +/- interposition bone wax / fat / fascia / vascularized graft
- +/- postoperative NSAIDS / radiation
Results
- excision of synostosis in 18 limbs
- no NSAIDS or irradiation postoperative
- recurrence in 1 patient with traumatic brain injury
- no evidence of efficacy of fat graft interposition
- possible better results with earlier surgery
Plate removal and refracture
Increased risk of refracture with routine plate removal
Yao et al Arch Orthop Trauma 2014
- 122 BBFF plating
- plate removal: refracture rate 13%, all low energy trauma
- plate retention: refracture rate 3%, all high energy trauma
- systematic review of plate removal and refracture
- lower risk of refracture with plate retention




