Definition
Pain / sensory disturbance / motor weakness in distribution of a cervical nerve root
Impingement of exiting nerve roots
- herniated nucleus pulposis (HNP)
- facet joint hypertrophy
Epidemiology
- 4th decade of life
- men
- cigarette smoking
- occupations with driving / vibrating equipment
Natural History
- systematic review of natural history of cervical radiculopathy
- substantial improvement in 4 - 6 months
- complete recovery in 83% of patients in 2 - 3 years
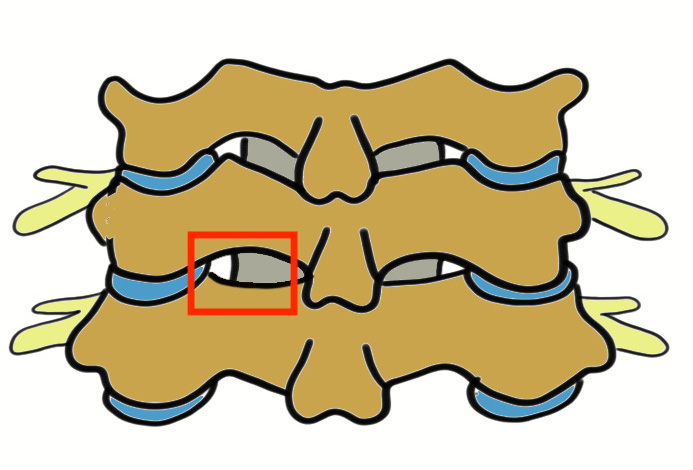
Anatomy
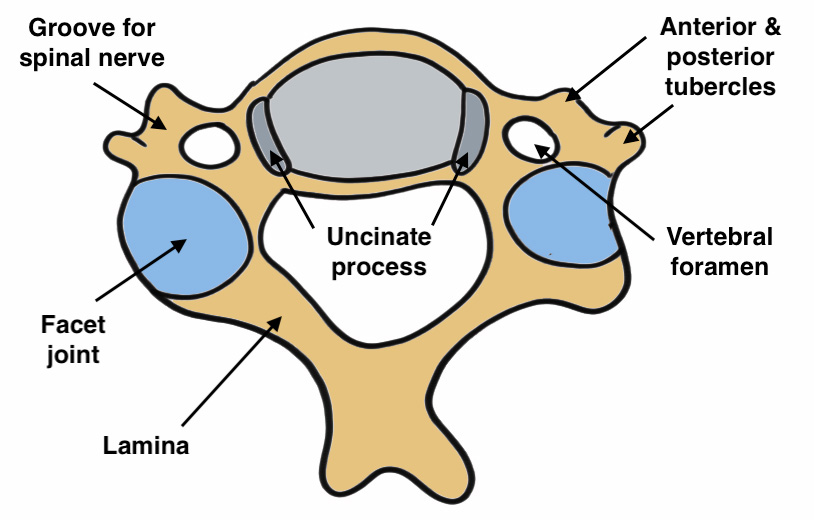
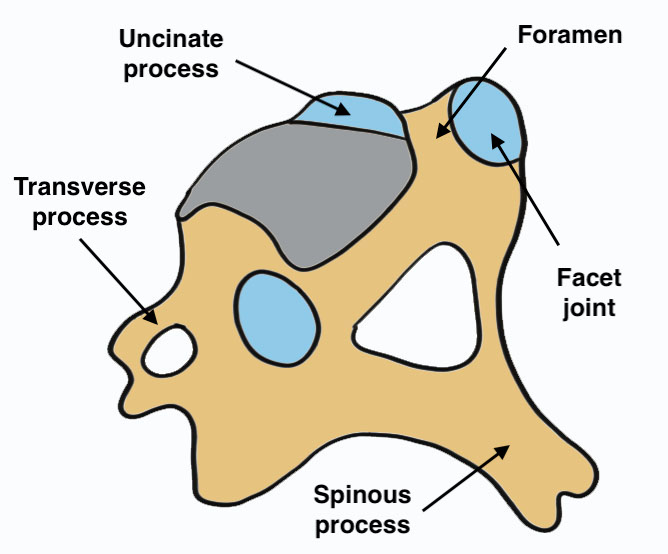
Each subaxial C-spine motion segment has 5 articulations
A. Intervertebral disc
B. Two uncovertebral joints
- joint of Luschka
- along posterolateral vertebral body
- lie between disc & nerve root
C. Two facet joints - angulated 30-50° to transverse plane
Intervertebral foramina boundaries
A. Anterior - vertebral bodies, vertebral disc, uncinate process & disc
B. Posterior - facet joints
C. Above & below - pedicles
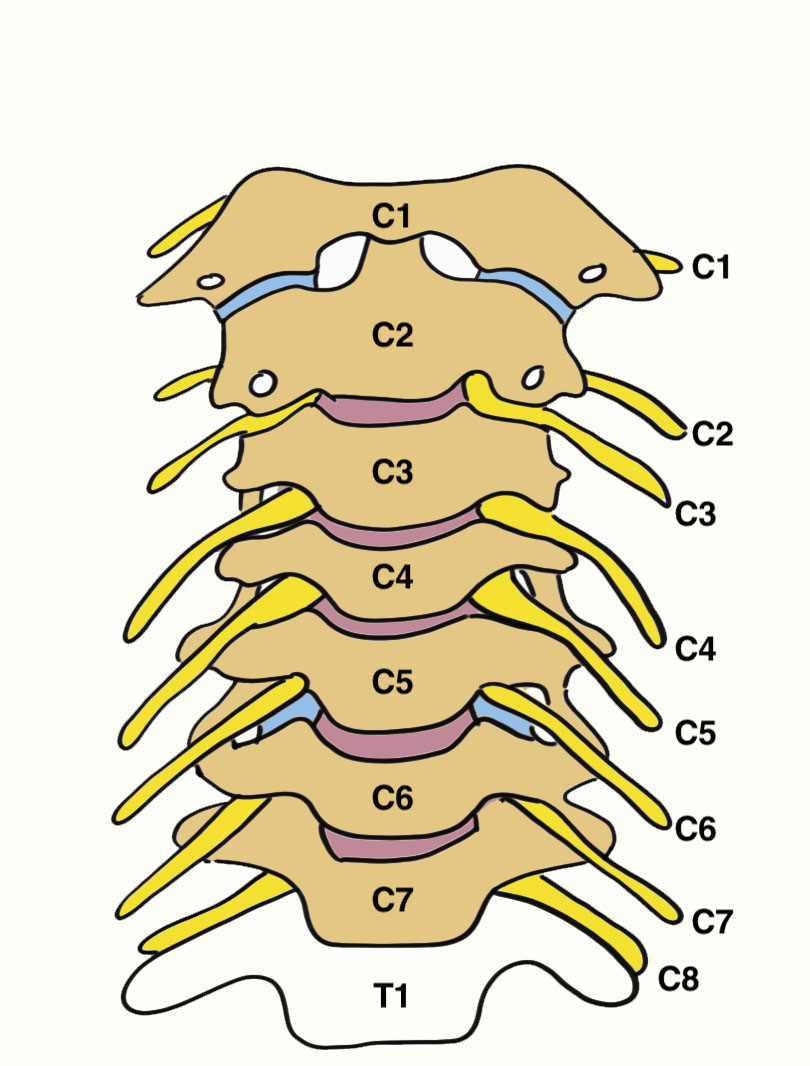
Cervical Nerve Roots
Each cervical root exits above the pedicle for which it is named except C8
- C5/6 – C6
- C6/7 – C7
- C7/T1 – C8
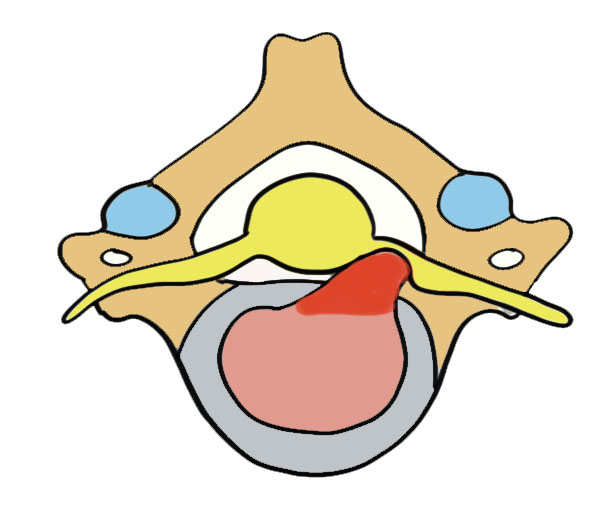
Causes of nerve root compression
1. Herniated nucleus pulposis (HNP)
- in contrast to lumbar spine both posterolateral and central HNP compress exiting nerve root
A. Central - myelopathy
B. Posterolateral - mainly motor weakness
C. Intraforaminal - most common / often dermatomal distribution
2. Bony impingement on nerve root foramen
A. Uncovertebral osteophytes / hard discs
B. Superior articular facet osteophytes
2. Spondylosis / Disc degeneration
- loss of height causes foraminal compression
History
Pain / parasthesia in distribution of nerve root
Examination
Spurling's test
Hyperextension with tilt toward affected side
- stimulates radiculopathy symptoms
- systematic review of examination for cervical radiculopathy
- Spurling's test high specificity (0.9 - 1.0) but variable sensitivity
Nerve root signs
| Nerve root | Sensory | Motor weakness | Affected Reflex |
|---|---|---|---|
| C2 | Occipital headaches | ||
| C3 | Occipital headaches | ||
| C4 | Neck pain | Scapular winging | |
| C5 | Shoulder and upper arm pain and numbness |
Deltoid Biceps |
Biceps |
| C6 | Radial forearm and thumb |
Wrist extension |
Brachioradialis |
| C7 | Middle finger |
Triceps Wrist flexion |
Triceps |
| C8 | Ring and little finger | Finger flexors | |
| T1 | Axillary numbness | Intrinsics | Horner's syndrome |
DDx
Nerve entrapment syndromes
Thoracic outlet syndrome
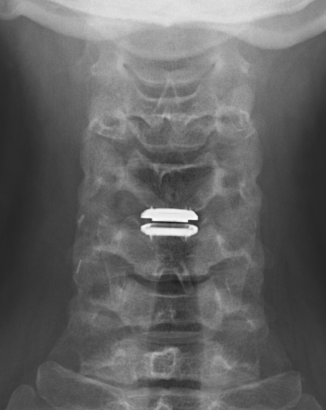
MRI
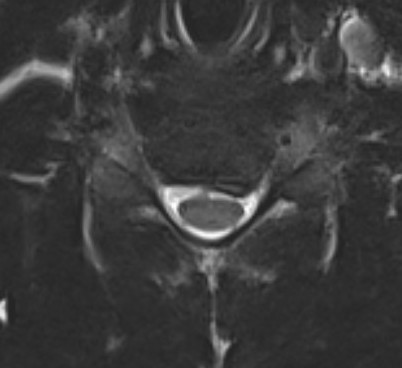
Paracentral disc
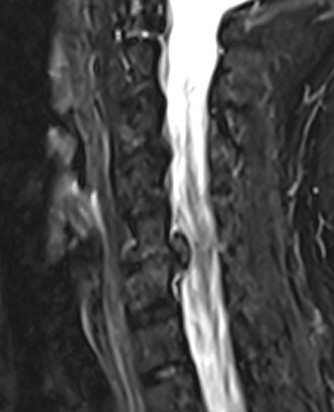
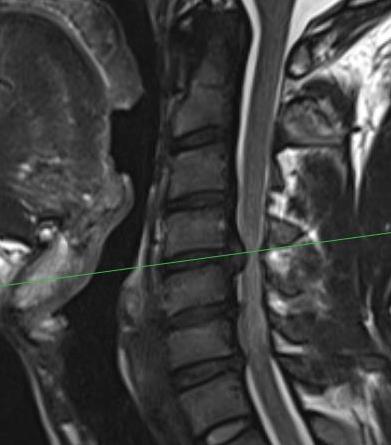
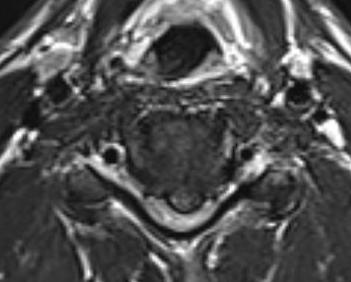
Foraminal disc
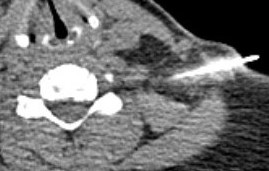
CT
May add complementary information to MRI
- posterolateral impingement from uncovertebral spur
- ossification of the PLL
EMG / NCS
Exclude peripheral nerve entrapment
Management
Operative versus nonoperative management
Luyao et al Global Spine J 2022
- systematic review of operative v nonoperative at one year for cervical radiculopathy
- improved neck pain, arm pain and NDI scores at all time periods for operative care
- faster pain resolution with surgery versus nonoperative care
Nonoperative Management
Options
Rest
NSAIDS
Physiotherapy +/- traction
Injections
Physiotherapy +/- traction

- meta-analysis of 10 RCTs looking at exercises for cervical radiculopathy
- improved VAS scores and reduced disability with exercises
- meta-analysis of 5 RCTs with regards use of traction
- mechanical traction improved pain at short and intermediate term
- manual traction improved pain at short term
Cortisone injections
Options
- transforaminal injections with CT
- interlaminar injections with CT
- ultrasound guided nerve blocks
Operative
Indications
Severe pain
Severe neurological impairment
Failure non operative treatment
Options
Anterior Cervical Discectomy (ACD)
Anterior Cervical Disc and Fusion (ACDF)
Anterior Cervical Disc Arthroplasty (ACDA) / Disc Replacement
Posterior Cervical Laminoforaminotomy (PCF)
Results
ACD versus ACDF
- systematic review of 21 RCTs and 1500 patients with cervical radiculopathy
- worse outcomes for anterior cervical discectomy without addition of intervertebral spacer / fusion
Fusion (ACDF) versus disc replacement (ACDA)
Goedmakers et al Eur Spine J 2020
- meta-analysis of ACDF versus ACDA for cervical radiculopathy secondary to herniated disc
- 8 studies
- no difference in clinical outcomes
- meta-analysis of 8 studies of ACDF versus ACDA
- improved outcomes with disc replacement with regards neck and arm pain
- lower complications and secondary surveys with disc replacement
- 5 year follow up of RCT of 109 patients
- ACDF versus ACDA for cervical radiculopathy secondary to herniated disc
- no difference in outcomes between fusion and arthroplasty
- no difference in adjacent level degeneration
Fusion (ACDF) versus posterior laminoforaminotomy (PCF)
- systematic review of minimally invasive PCF versus ACDF
- 14 studies with 1216 patients
- similar outcomes with regards neck pain
- improved arm pain with MIS - PCF
- no difference complications / reoperation rate
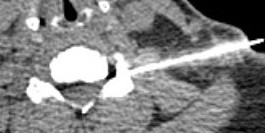
ACDF / Fusion


Technique
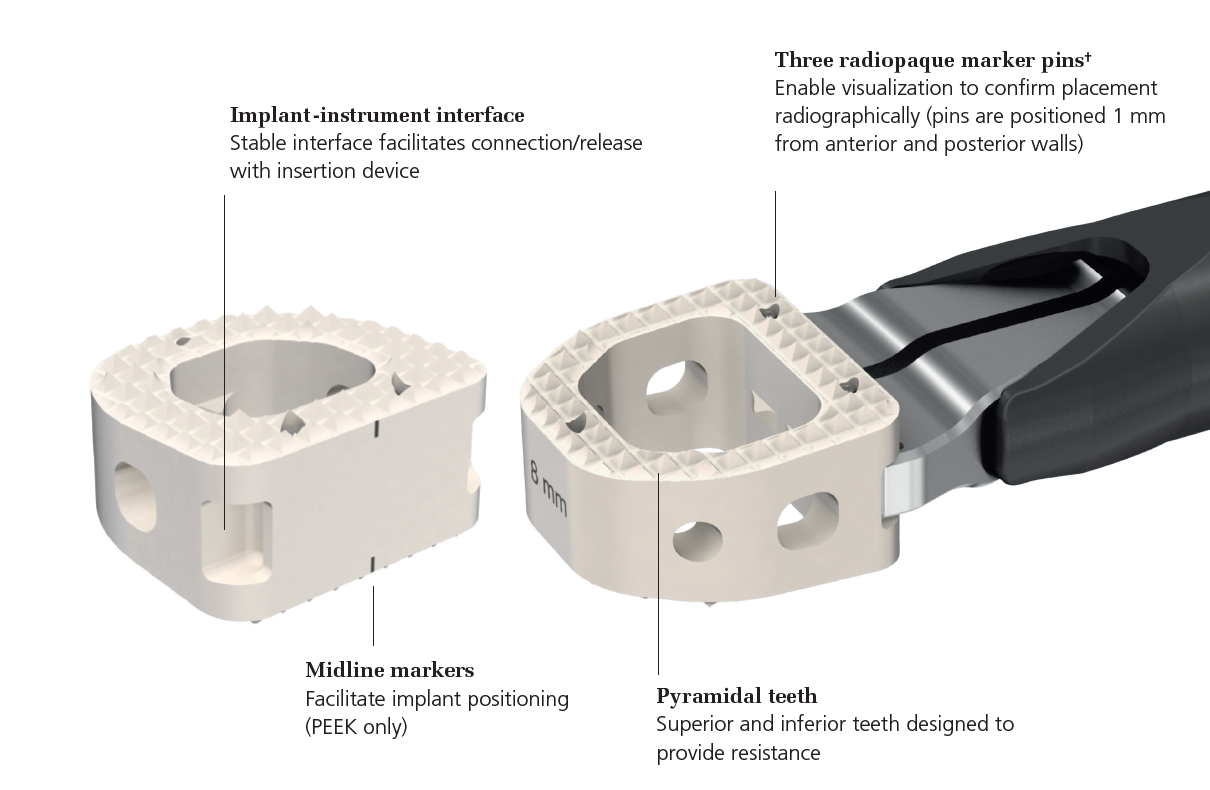
Depuy Synthes surgical technique article
Vumedi anterior discectomy technique
Anterior approach / Smith Robinson
- discectomy
- decorticate end plates
- interbody fusion with bone graft +/- interbody spacer
- anterior plate / integrated cage
Complications
Risks of Smith Robinson / Anterior Cervical Approach
Specific
- pseudarthrosis 0 - 4.3%
- hardware failure
- insufficient decompression
- degeneration at second level
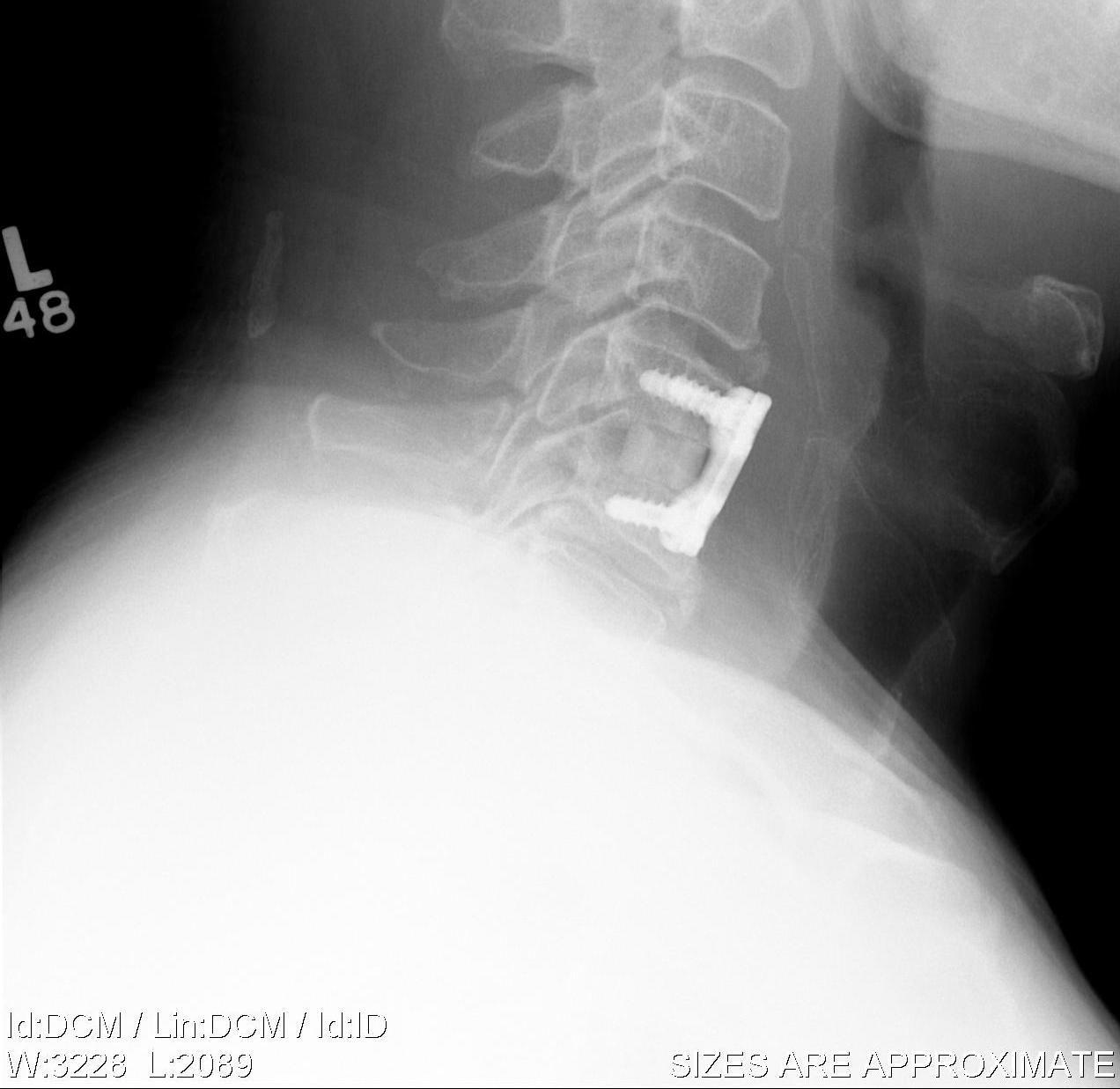
ACDA / Disc replacement

Advantage
Theoretically maintain some motion and preserve other disc segments
Contra-indications
Instability / Severe deformity / kyphosis - risk prosthesis displacement
Osteoporosis - risk of subsidence
Facet joint arthropathy - continued pain with disc motion
Technique



Depuy Discover Medtronic Prestige
Vumedi disc replacement technique
You tube prodisc C surgical technique animation
Complications
Risks of Smith Robinson / Anterior Cervical Approach
Specific
- anterior displacement
- posterior displacement and spinal cord injury
- subsidence 3% - higher risk if remove or disrupt end plates
- osteolysis
- implant failure
- heterotopic ossification
- meta-analysis of HO after disc replacement
- 38% at 1-2 years, 54% at 5-10 years
- severe HO 11% at 1-2 years, 48% at 5 - 10 years
Posterior Cervical Laminoforaminotomy (PCF)
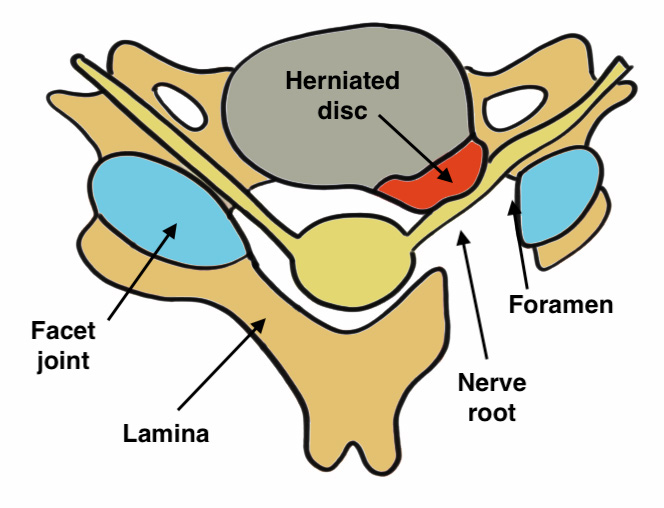
Indication
Foraminal stenosis
Laterally located disc
Rarely used
Options
Open
Minimally invasive (MIS) - tube retractor and microscope
Endoscopic
Technique
Youtube animation of cervical laminoforaminotomy
Vumedi MIS Cervical Foraminotomy
Endoscopic Cervical Foraminotomy Technique article
Posterior approach
- laminotomy
- decompress foramin
- discectomy
Results
- meta-analysis of open versus MIS PCF
- no difference in clinical success rate (95% MIS, 93% open)
- systematic review of MIS versus endoscopic PCF
- no difference in clinical success rate (90% MIS, 94% endoscopic)
- increased dural tears with MIS
- increased transient nerve root palsy with PCF