Epidemiology
Third most common fracture after hip and distal radius
70% in patients aged 60 years or older
Etiology
Elderly patients - osteoporosis
Young patients - high energy trauma
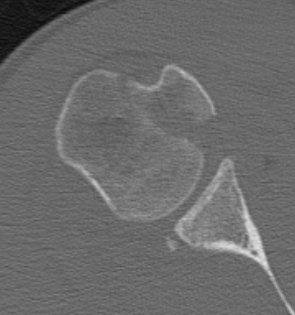
Anatomy
Surgical neck - junction of diaphysis and metaphysis
Anatomical neck - junction of head and metaphysis
Neck shaft angle 130o
Head retroverted 20o relative to shaft
Blood supply
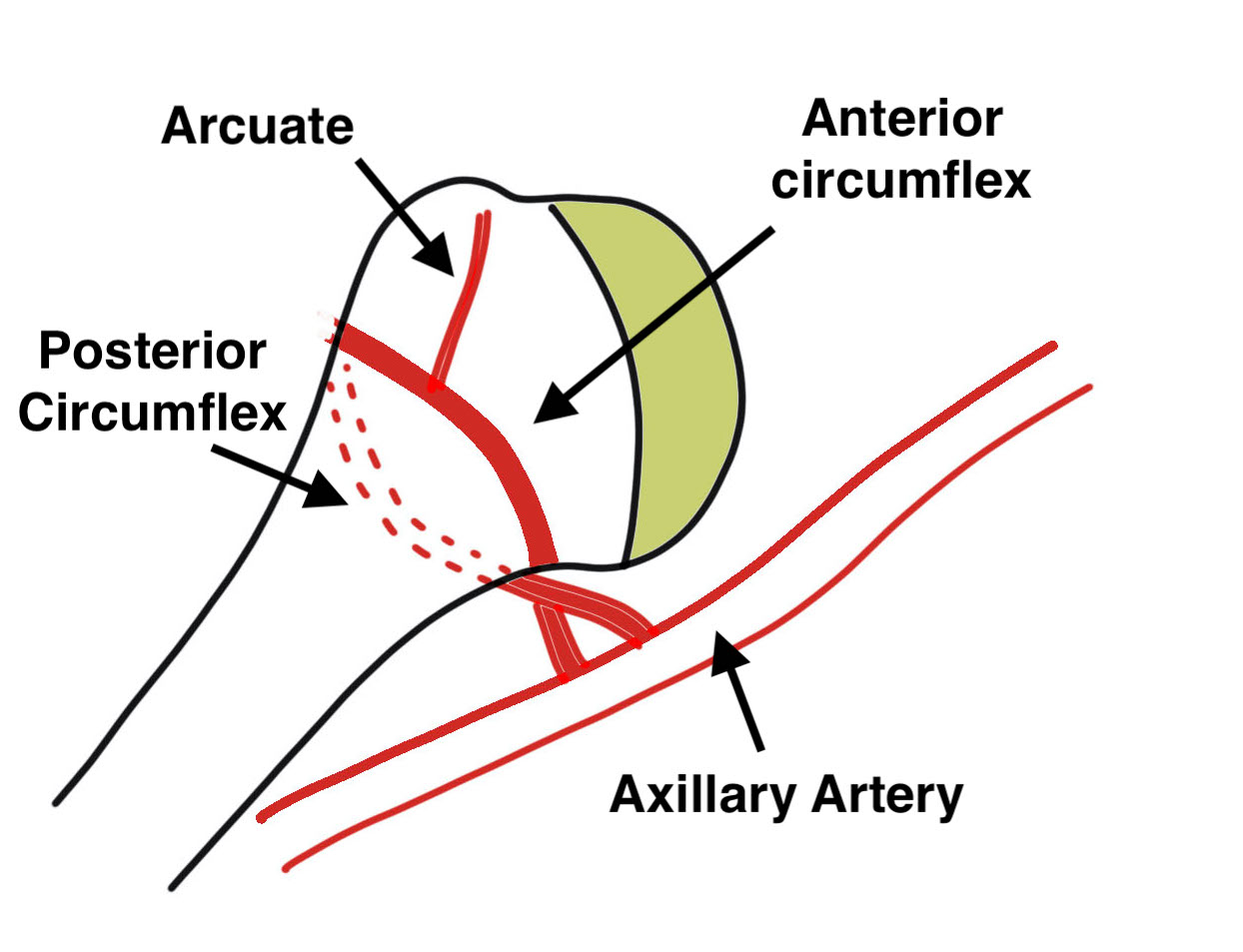
| Anterior humeral circumflex | Posterior Humeral circumflex | Rotator cuff |
|---|---|---|
| Major supply
Anterolateral branch |
Small contribution posterior head Allows head to survive with both tuberosities fractured |
Supplies blood to tuberosities in fractures |
| Nearly always disrupted in fractures |
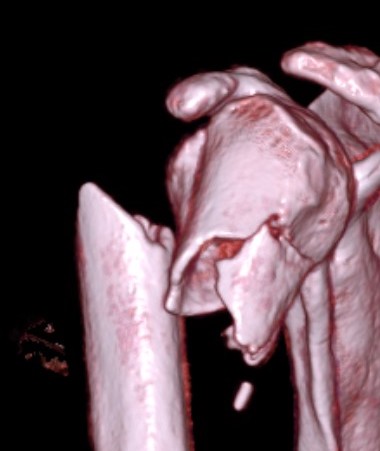
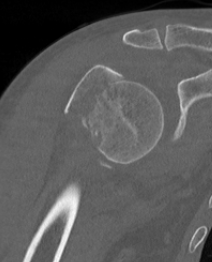
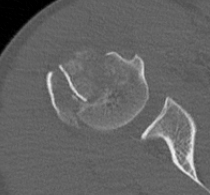
Neer Classification
Displaced fragments - > 1 cm displaced and/or > 45o angulated
Number of parts - 2, 3 or 4
| Two part | Three part | Four part |
|---|---|---|
|
Surgical neck fracture Anatomical neck fracture Greater tuberosity fracture Lesser tuberosity fracture |
Surgical neck + greater tuberosity Surgical neck + lesser tuberosity |
Surgical neck + greater tuberosity + lesser tuberosity |
| Fracture dislocations |
Fracture dislocations Head split |
Fracture dislocations |
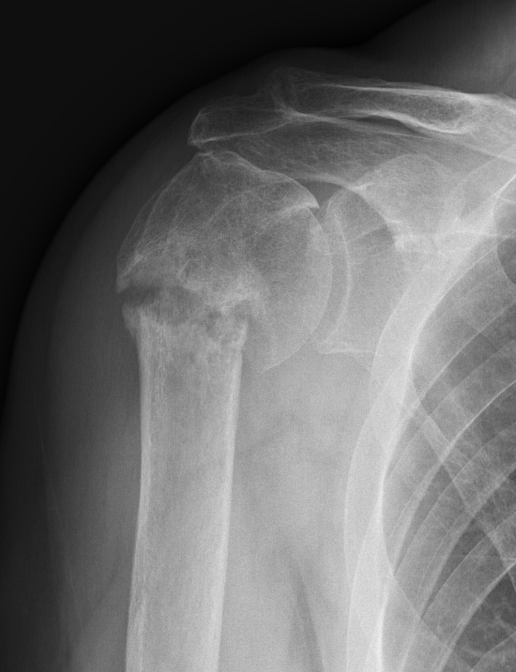
Two part


Displaced greater tuberosity fracture

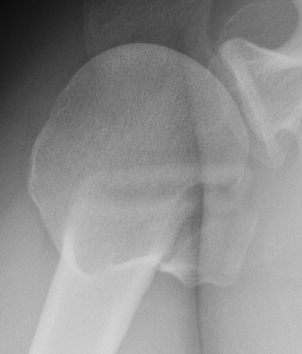
Displaced lesser tuberosity fracture

Two part proximal humerus fracture


Two part proximal humerus fracture dislocation posterior
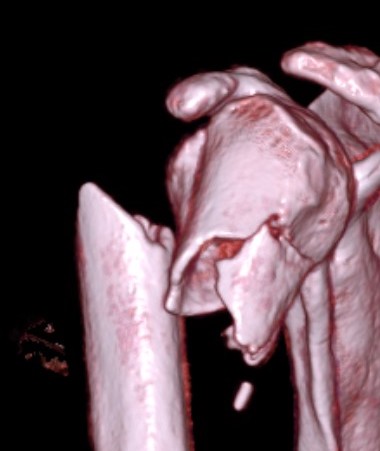
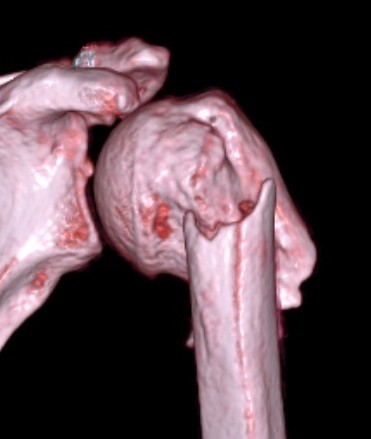
Three part

Three part with greater tuberosity fracture



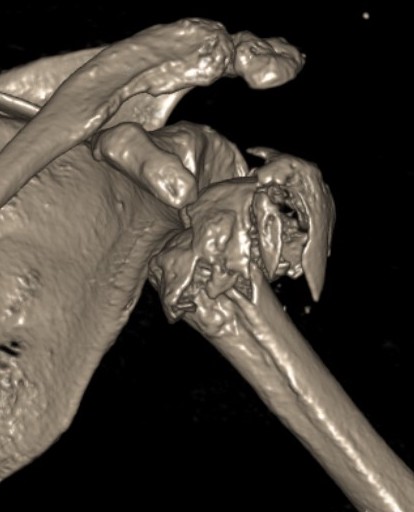
Three part fracture dislocation anterior


Three part fracture dislocation with anatomical neck


Three part head splitting fracture
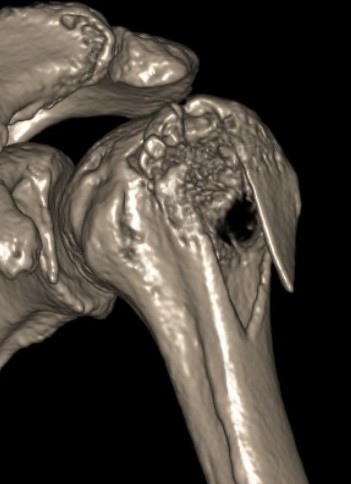
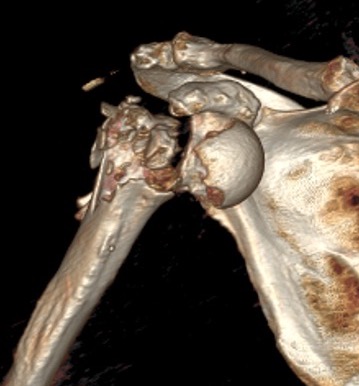
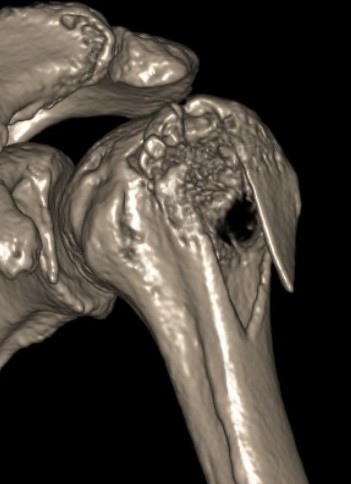
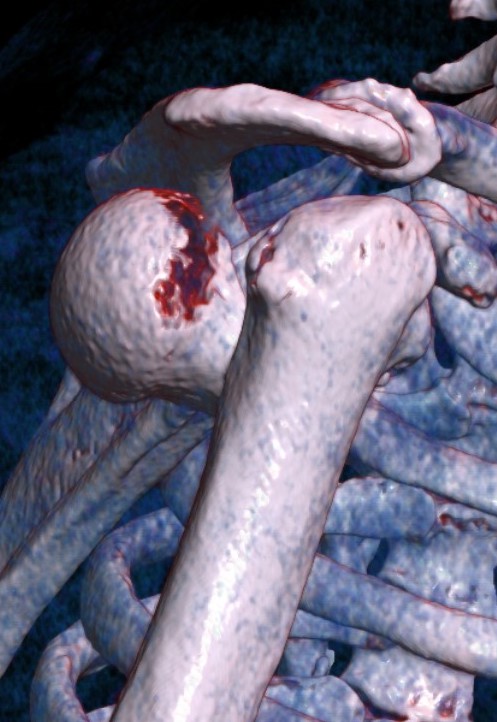
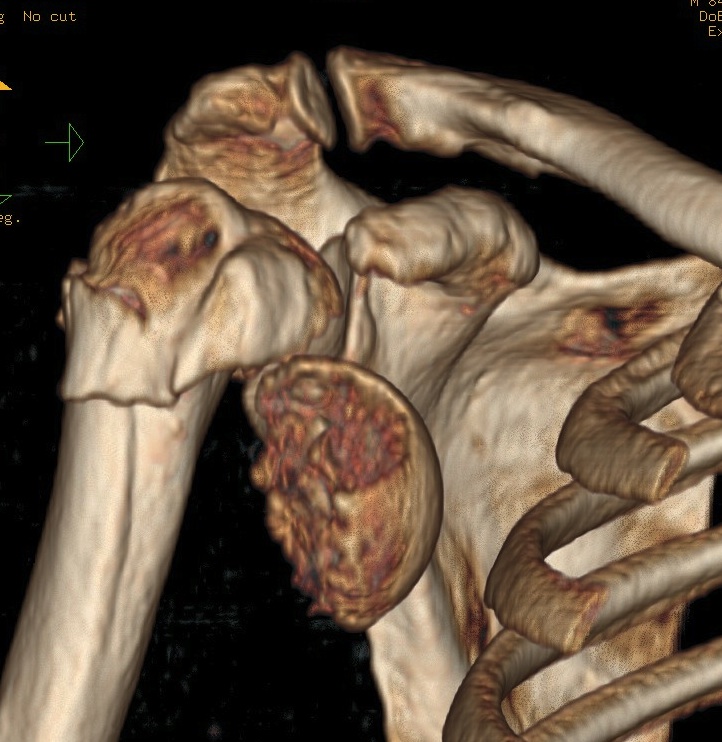
Four part




Avascular necrosis (AVN)

In most fractures, arcuate artery is disrupted, but head survives
- posterior circumflex artery is sufficient
- risk increases with amount of displacement
- 4 part fracture 30%
- 3 part fracture 15%
Hertel et al J Should Elbow Surg 2004
- two criteria to predict ischaemia / 97% predictive if both factors present
- metaphyseal head extension < 8 mm
- medial hinge displaced > 2mm
Deforming Forces
| 2 part fracture | Greater tuberosity fracture | Lesser tuberosity fracture |
|---|---|---|
|
Pectoralis major displaces shaft medially Head internally rotated by SSC |
Fragment pulled postero-superior Combination of supraspinatus / infraspinatus / Teres minor |
Displaced medially by subscapularis |
 |
 |
 |
Management
Options
Nonoperative
Operative - ORIF (plate, IMN), hemiarthroplasty, reverse TSA
Operative versus non operative
Nonoperative versus ORIF / Hemiarthroplasty
- PROFHER trial
- 250 patients RCT of nonoperative versus ORIF/hemiarthroplasty
- mean age 66 (range, 24 - 92)
- 215 patients
- no difference in functional outcomes
- RCT of 160 patients nonoperative v ORIF v hemiarthroplasty
- > 60 years and displaced 3 or 4 part SNOH
- non difference in functional outcomes
- complications: nonoperative 6%, ORIF 45%, hemiarthroplasty 10%
Nonoperative versus Reverse TSA
- RCT of 81 patients rTSA v nonoperative
- > 70 years and displaced 3 or 4 part SNOH
- 8 point better Constant score with rTSA
Nonoperative versus ORIF
- RCT of 88 patients nonoperative versus ORIF
- > 60 years and displaced 2 part SNOH
- no difference in outcomes
Operative management
Intra-medullary nail versus ORIF with plate
- RCT of 85 patients ORIF v IMN
- mean age 74 years and displaced 3 or 4 part SNOH
- better outcome scores and lower complications with IMN
- systematic review of ORIF v IMN
- IMN shorter OR times and blood loss
- similar functional outcomes and complication rates
Reverse TSA versus ORIF with plate
- DelPhi trial
- RCT of 124 patients rTSA v ORIF
- > 65 years and displaced 3 or 4 part SNOH
- 14 point better Constant score with rTSA
Reverse TSA versus hemiarthroplasty
- RCT of 99 patients rTSA v hemiarthroplasty
- > 70 years and displaced 3 or 4 part SNOH
- 10 point better Constant score with rTSA
- better ROM with rTSA: abduction 110 v 80, flexion 125 v 90
Nonoperative treatment
Rehabilitation
Challoumas et al BMC Musculoskeletal 2025
- 1 week sling v 3 - 4 week sling immobilization
- meta-analysis of 6 RCTs
- no difference in outcome
- better at 3 months with early ROM
Non-union

Options
- ORIF + fibular strut
- reverse TSA
Malunion


- systematic review of early versus delayed rTSA for SNOH
- better ROM and outcome scores with early rTSA
- increased complication rate with delayed rTSA
