

Epidemiology
Bimodal
Young patients - high velocity injuries
Older patients - low velocity / osteoporosis
Anatomy
| 3 columns | Three articular surfaces |
|---|---|
|
Radial column with scaphoid fossa and radial styloid
Intermediate column with lunate fossa and sigmoid notch
Ulna column with TFCC and distal ulna |
Scaphoid facet
Lunate facet
Sigmoid notch |
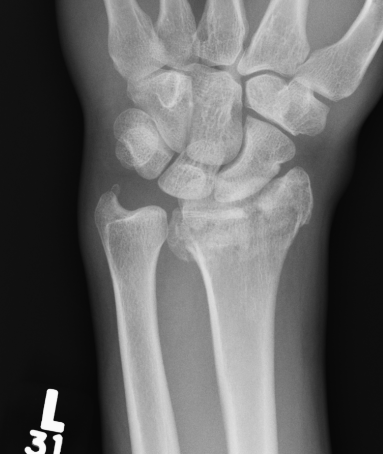
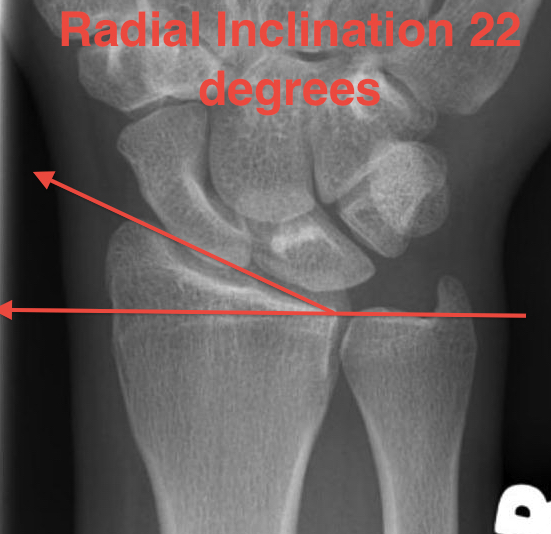
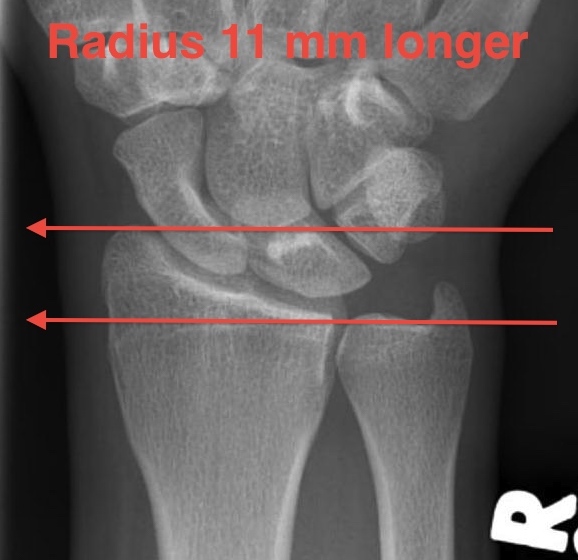
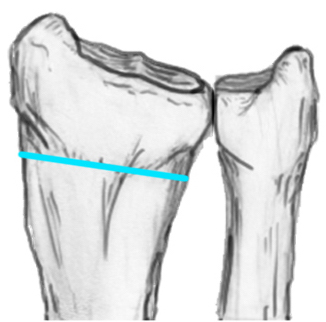
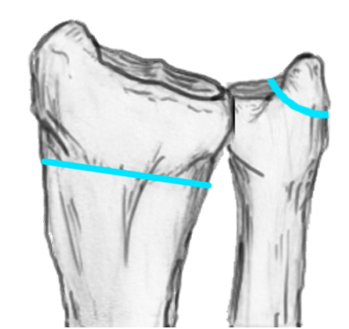
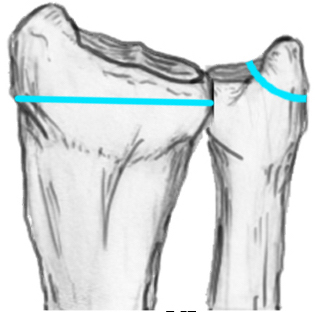
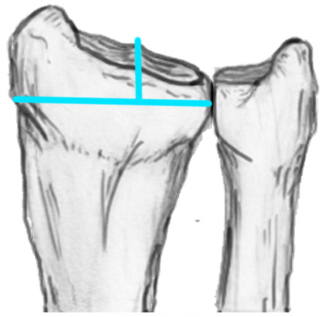
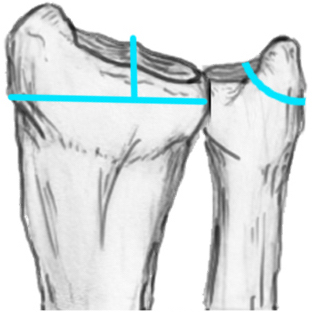
Radial angles
| Volar tilt mean 11° | Radial inclination mean 22° | Radius mean 11 mm longer than ulna |
|---|---|---|
 |
 |
 |
Fracture Patterns
Frykman Classification
| Type I | Type II | Type III | Type IV |
|---|---|---|---|
| Extra-articular fracture |
Extra-articular fracture + ulna styloid |
Intra-articular fracture |
Intra-articular fracture + ulna styloid |
 |
 |
 |
 |
| Type V | Type VI | Type VII | Type VII |
|---|---|---|---|
| Transverse fracture into DRUJ |
Transverse fracture into DRUJ + ulna styloid |
Intra-articular fracture + DRUJ |
Intra-articular fracture + DRUJ + ulna styloid |
 |
 |
 |
 |
Named fracture patterns
| Colle's fracture | Smith's fracture | Chauffeur's Fracture |
|---|---|---|
| Distal radius fracture with dorsal displacement | Distal radius fracture with volar displacement | Radial styloid fracture |
 |
 |
 |
| Volar Barton's fracture | Reverse Barton's fracture | Die Punch |
|---|---|---|
|
Volar intra-articular fragment Inherently unstable |
Dorsal intra-articular fracture | Depressed articular fragment |
 |
 |
|
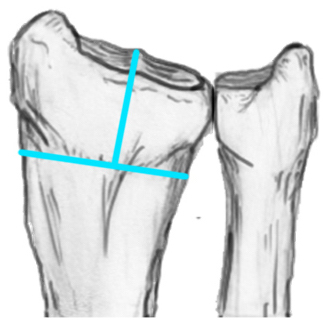
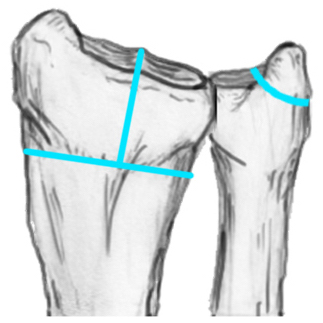
Fracture configurations
| Extra-articular fracture | Intra-articular with scaphoid and lunate fossa fragments | Volar Barton's |
|---|---|---|
 |
 |
 |
| Dorsal fractures | Volar ulnar fracture | Sigmoid notch involvement |
|---|---|---|
 |
 |
 |
Management
Reduction
Conscious sedation
- 2 minutes of traction / reduction of deformity
- backslab
- re-xray

Indications for surgery
Absolute
- open fracture
- acute severe carpal tunnel syndrome



Relative
1. Failure to obtain and maintain adequate reduction
- unclear, likely dependent on age
- radial shortening > 5 mm
- dorsal tilt > 15o
- articular incongruency > 2 mm
2. Unstable fracture patterns - volar Barton's, DRUJ
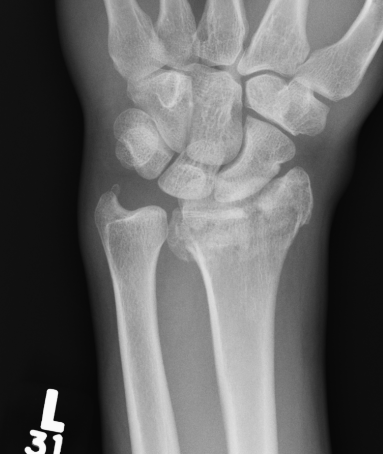

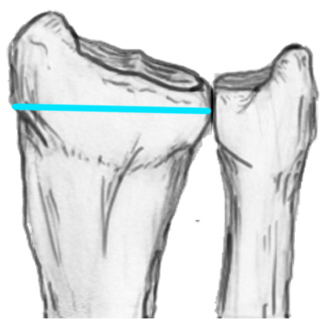
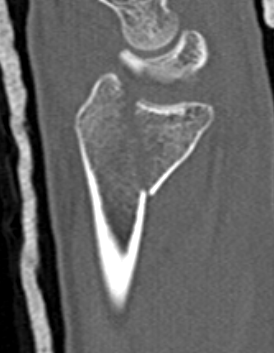
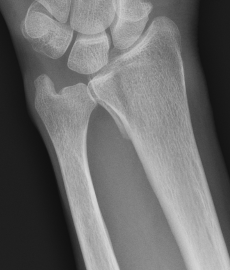
Distal radius fracture with shortening and dorsal tilt


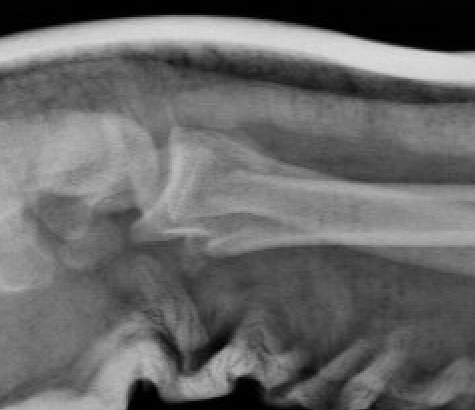
Articular incongruency > 2 mm


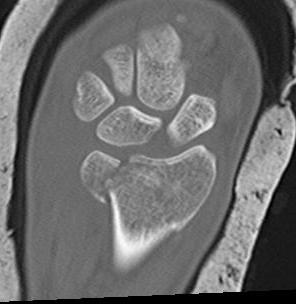
Sigmoid notch disruption and DRUJ instability
Operative versus non operative management
Outcomes
- systematic review of operative v nonoperative distal radius fractures
- 17 RCTs and 1700 patients
- improved outcome scores, grip strength and pronation / supination with surgery
- no difference in wrist flexion or extension
Patients > 60: It is likely that surgery in older patients is not related to improved outcomes
CROSSFIRE study JAMA Surg 2021
- RCT of 166 patients > 60
- closed reduction v volar plating
- no clinically important between group differences at 12 months
Latypov et al J Wrist Surg 2023
- systematic review of 6 RCTs displaced distal radius fractures > 60 years
- closed reduction versus volar plating
- DASH outcome better with surgery, but mean of 3/100 points which did not reach MCID
- no difference in complicatons
- systematic review of 6 RCTs and 550 patients > 60
- closed reduced v volar plating
- DASH outcome better with surgery, but mean of 6/100 points which did not reach MCID
Surgical options
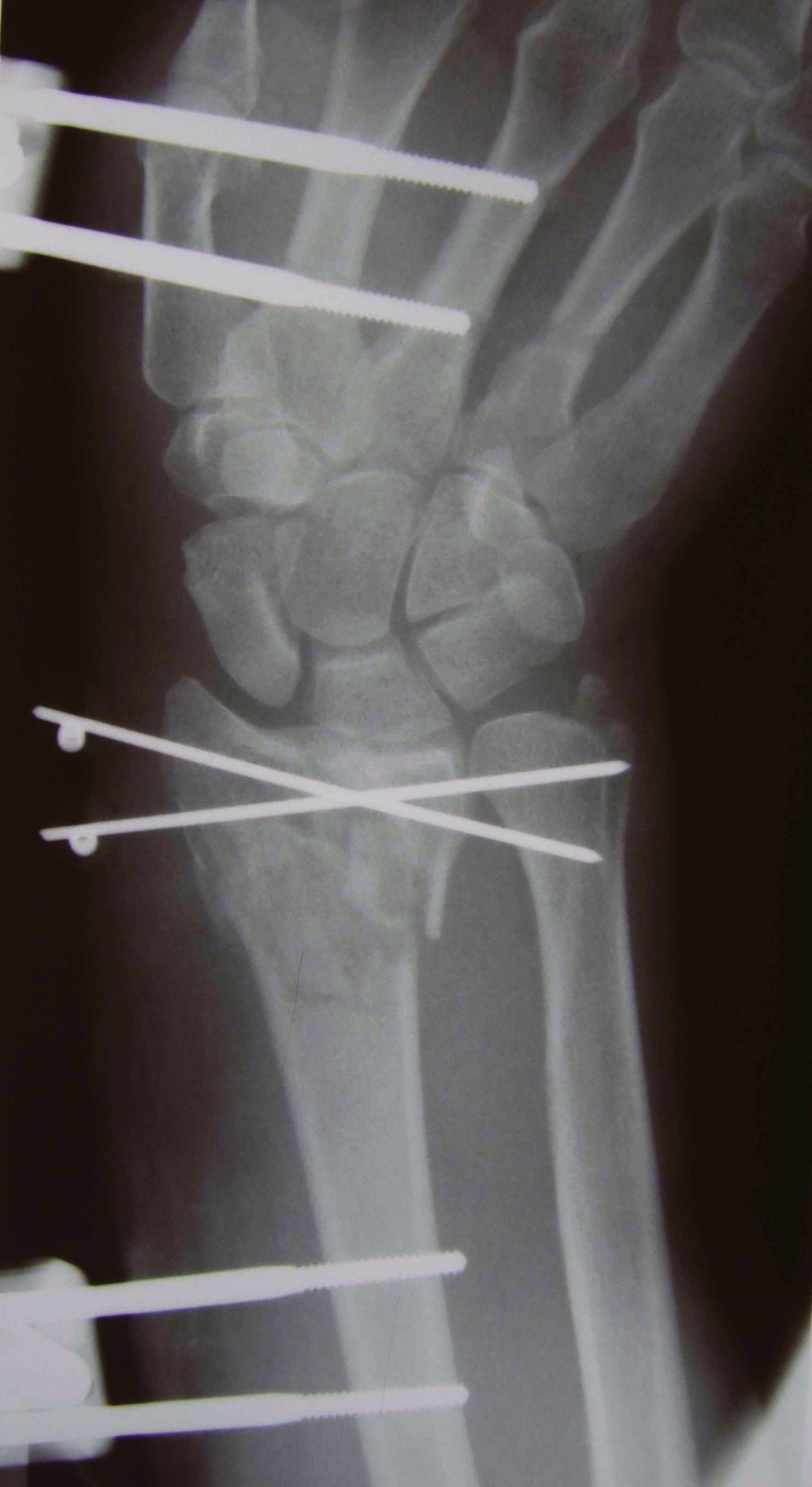
K wires
Volar locking plates
External fixation
Dorsal spanning plates



K wire v Volar locking plates
Francheschi et al Br Med Bull 2025
- systematic review of K wires v volar locking plates
- 14 studies and 1300 patients
- better DASH outcome scores with locking plates
- increased cost and surgical times with locking plates
Plates v External Fixation
Gou et al BMC Musculoskeletal 2021
- systematic review of external fixation versus volar locking plates
- 12 studies and 1200 patients
- better outcome scores and lower complications with volar locking plates

