
Conditions
Anterior sternoclavicular joint (SCJ) dislocation
Posterior sternoclavicular joint (SCJ) dislocation
Sternoclavicular joint septic arthritis
Sternoclavicular osteoarthritis
SAPHO
Condensing osteitis
Friedrich's Disease
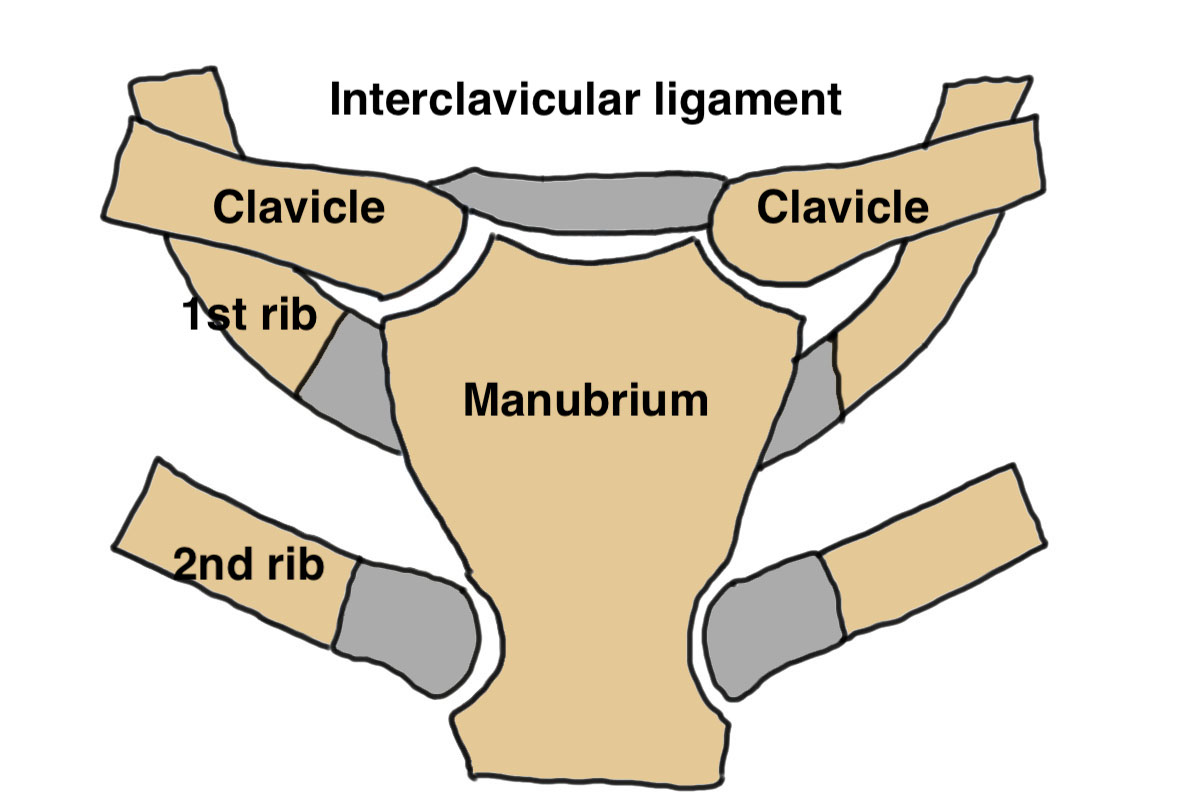
Anatomy
Medial clavicle physis is last to fuse aged 23 - 25
- can be medial clavicle physeal injury up to 25
Sternoclavicular joint
- synovial joint with a fibrocartilaginous disc
- only 50% of medial clavicle articulates with manubrium
- costoclavicular / interclavicular / sternoclavicular ligaments
Vascular
- brachiocephalic veins lie directly behind SCJ
- common carotid artery / subclavican artery / aortic arch / internal jugular vein very close
Anterior sternoclavicular dislocation
Epidemiology
9x more common than posterior SCJ dislocation
Mechanism
Traumatic
- lateral compression force
- disrupts anterior capsule but posterior capsule remains intact
Atraumatic
- ligament instability - hypermobility, Ehlers Danlos
Clinical
Imaging
Nonoperative management
Mainstay of treatment
- closed reduction has high rate of recurrence
- usually well tolerated
- systematic review of anterior SCJ dislocations
- 70% good or excellent results with nonoperative
- 92% good or excellent with closed reduction
Operative management
Indication
- recurrent instability
- pain / osteoarthritis
Options
Reduction and ligament stabilization
ORIF / fusion
Techniques
Vumedi anterior SCJ reconstruction video
Vumedi anterior SCJ reconstruction video 2
Arthroscopy techniques hamstring autograft SCJ stabilization PDF
OJSM Internal Bracing SCJ stabilization PDF
Results
- 22 shoulders undergoing SCJ hamstring autograft reconstruction
- minimum 5 year follow up
- 10% recurrent instability
- systematic review of 40 studies and 108 cases treated surgically
- 4% recurrent instability
- ligament reconstruction had lowest recurrence rate
- ORIF required hardware removal 80% of time
Posterior sternoclavicular joint dislocation
Mechanism
Direct blow to SCJ with posterior force
Posterior capsule is disrupted
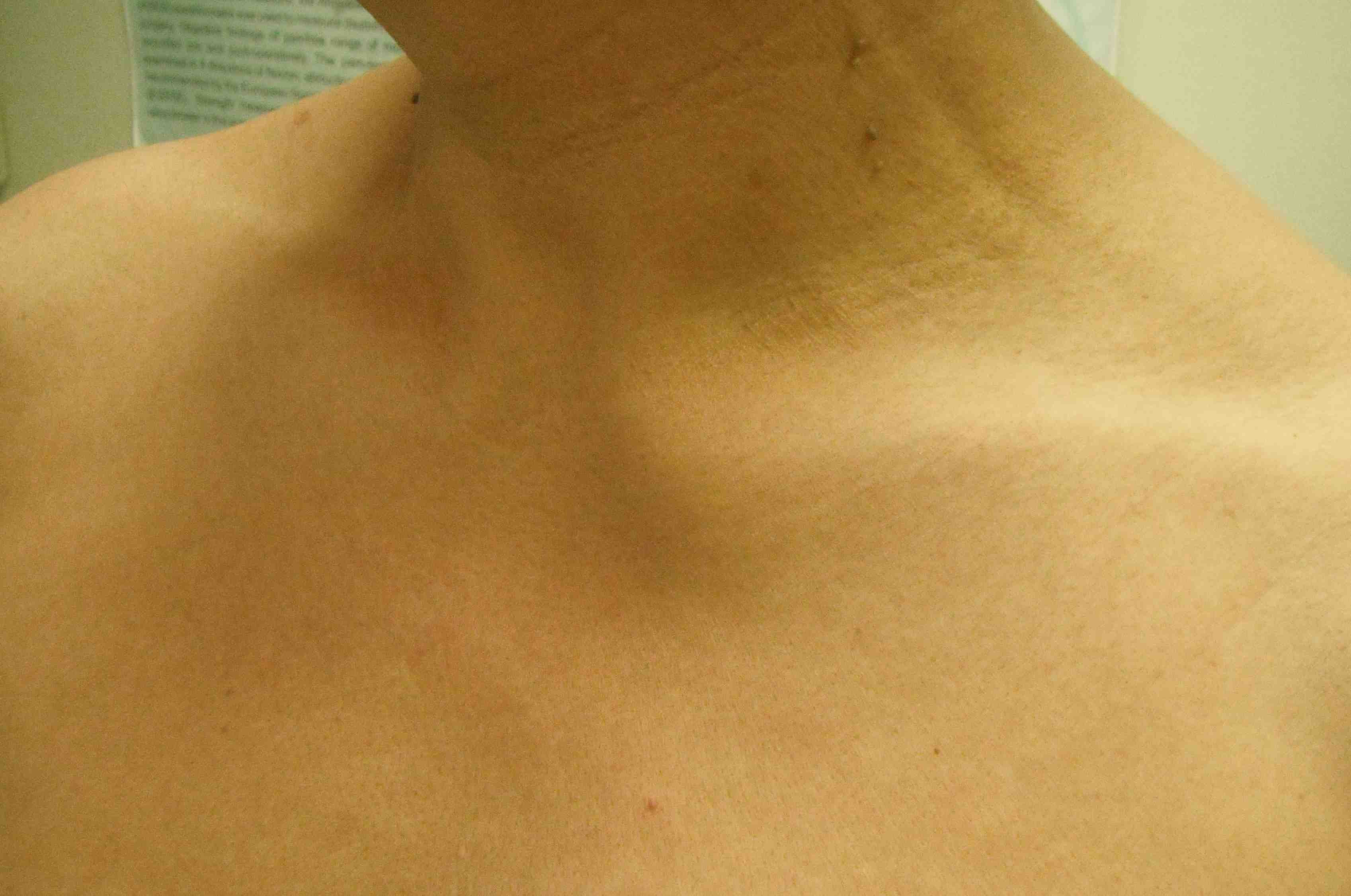
Clinical presentation
Can impinge on airway and posterior neurovascular structures
- shortness of breath
- difficulty swallowing / dysphagia
- neurological or vascular compromise -
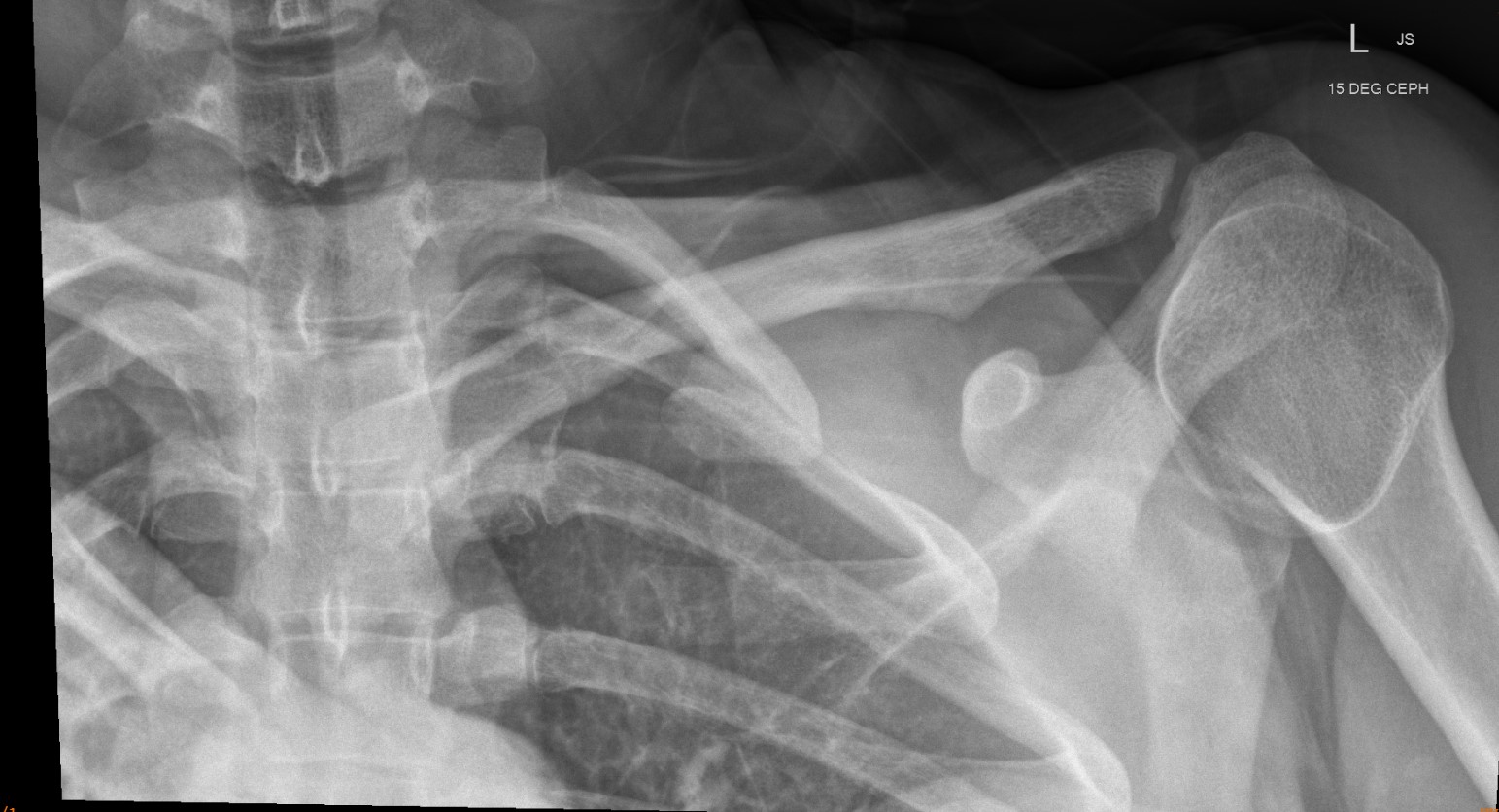
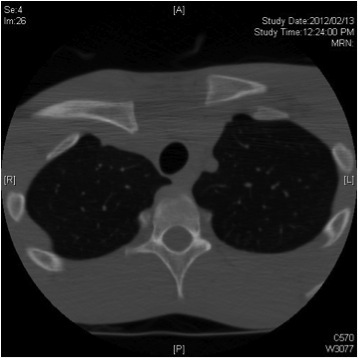
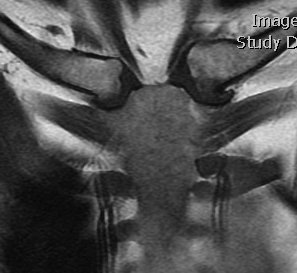
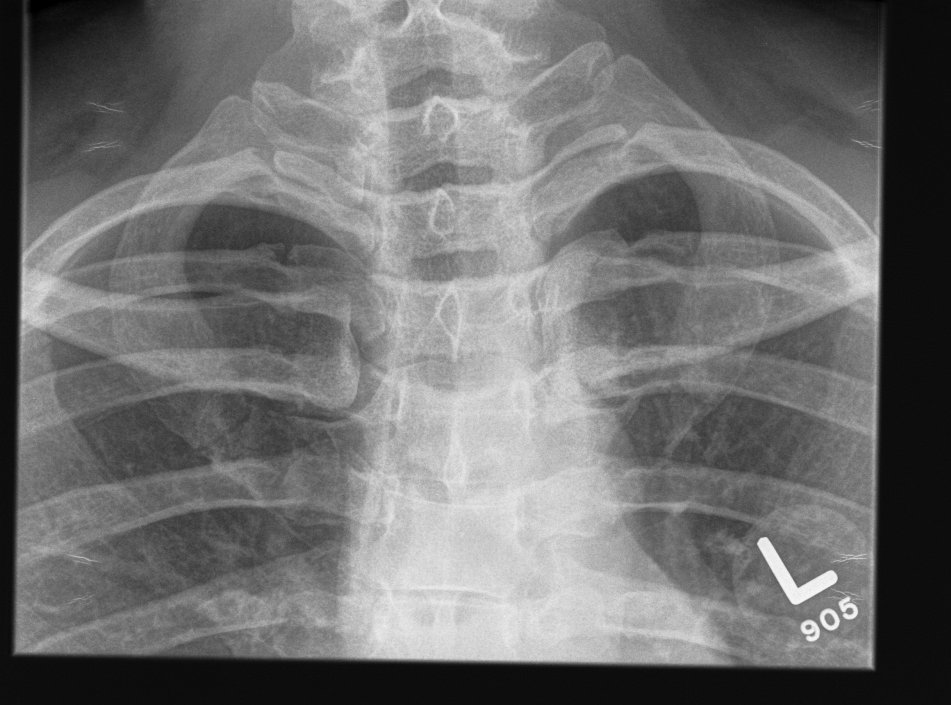
Xray
Can be missed on a xray

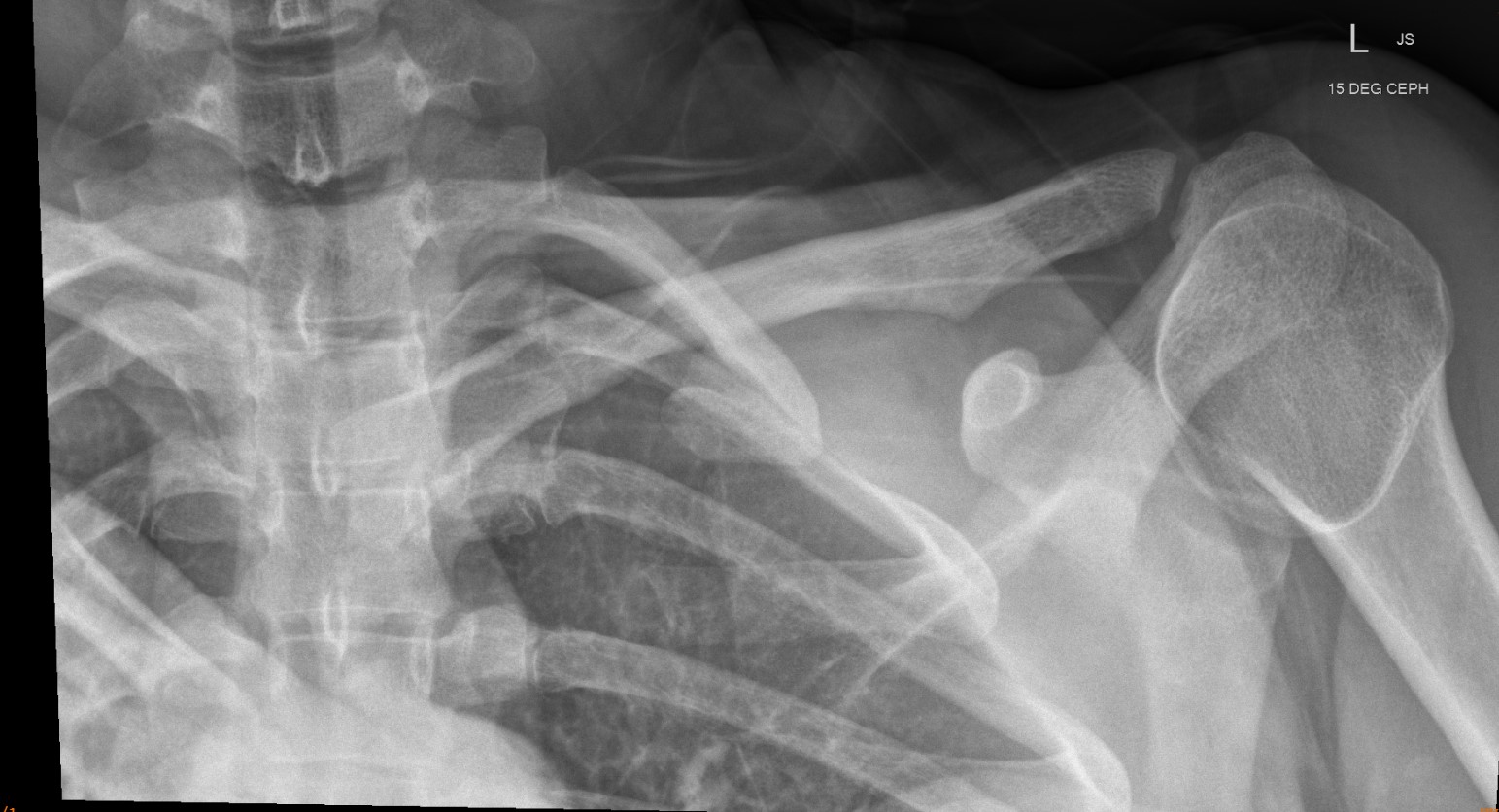
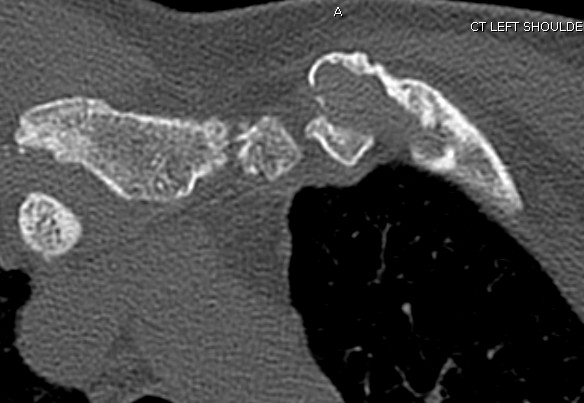
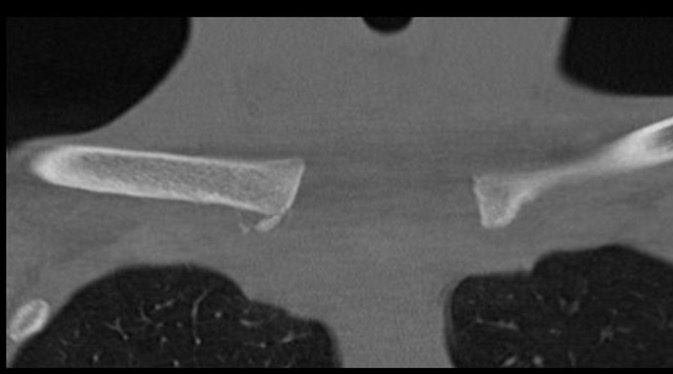
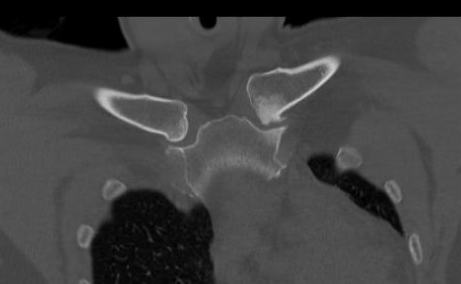
CT scan


Left posterior SCJ dislocation with pre- and post angiogram

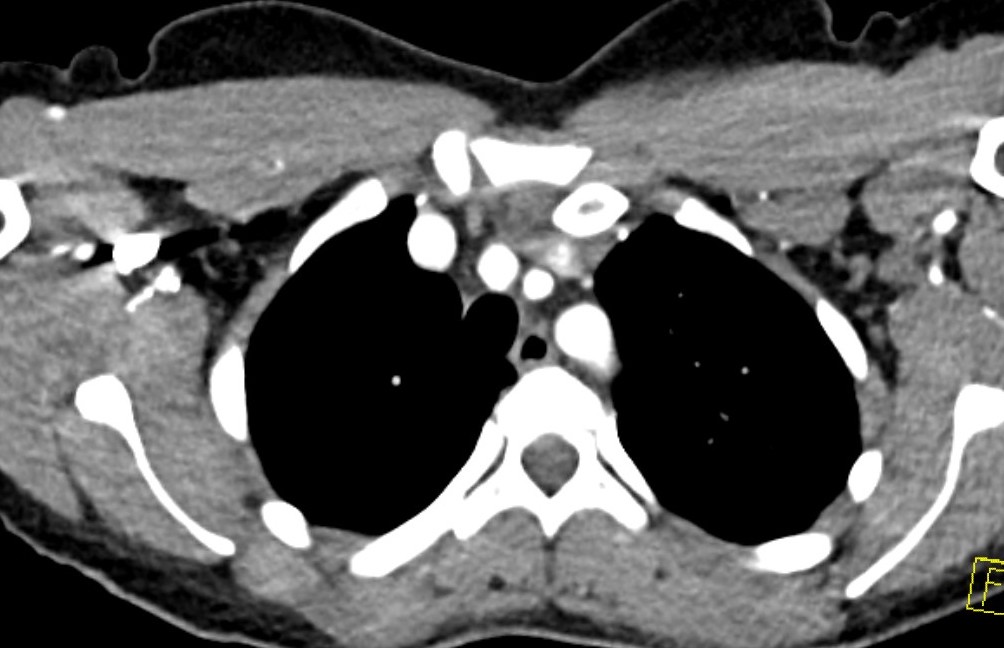
Left posterior SCJ dislocation with pre- and post angiogram


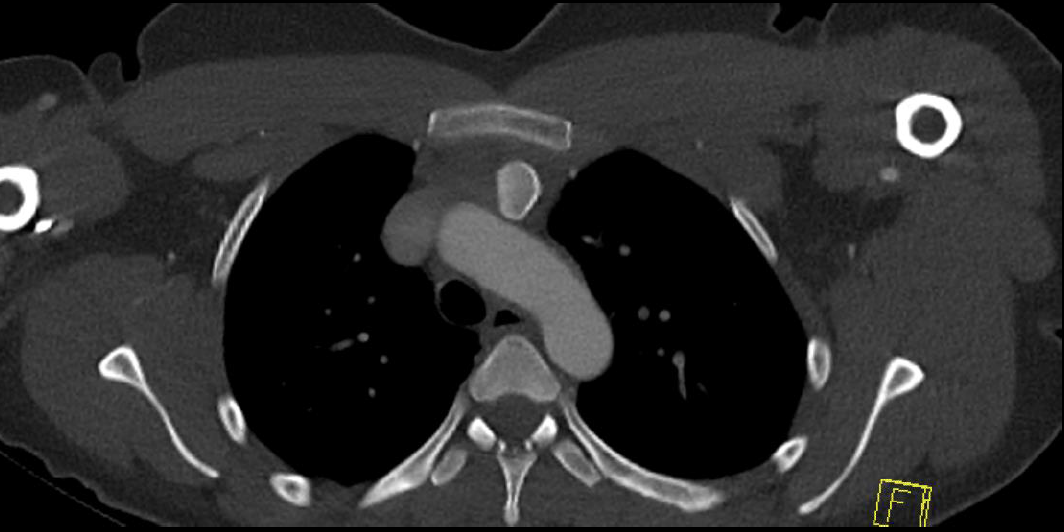
Severe left posterior SCJ dislocation with subclavian vein compression
Adolescent
Can be medial clavicle physeal injury up to age 25

Management
Cardiothoracic surgeon available in case vascular injury occurs
1. Closed reduction
A. Lateral traction on abducted arm with anterior directed shoulder force
B. Towel clip on medial clavicle
Lee et al J Pediatr Orthop 2014
- 48 adolescent posterior SCJ dislocations
- half true dislocations, half medial clavicle physeal injury
- 17% successful closed reduction
- 14 closed reductions
- successful in 5/14 (36%)
- failed in all medial physeal fracture dislocations
2. Open reduction
Performed under GA in operating room
- chest surgeon available
- potential vascular / airway catastrophe associated with injuries to the mediastinum
- thorough vascular imaging pre-operatively
3. Assess stability
Successful closed reduction usually stable
Unstable after reduction
- stabilize
- graft reconstruction / intra-osseous sutures / anchors / ORIF with bridging plate / sternoclavicular hook plate
Technique
Vumedi posterior SCJ reduction and hamstring allograft stabilization video
Vumedi chronic posterior SCJ reduction and reconstruction video
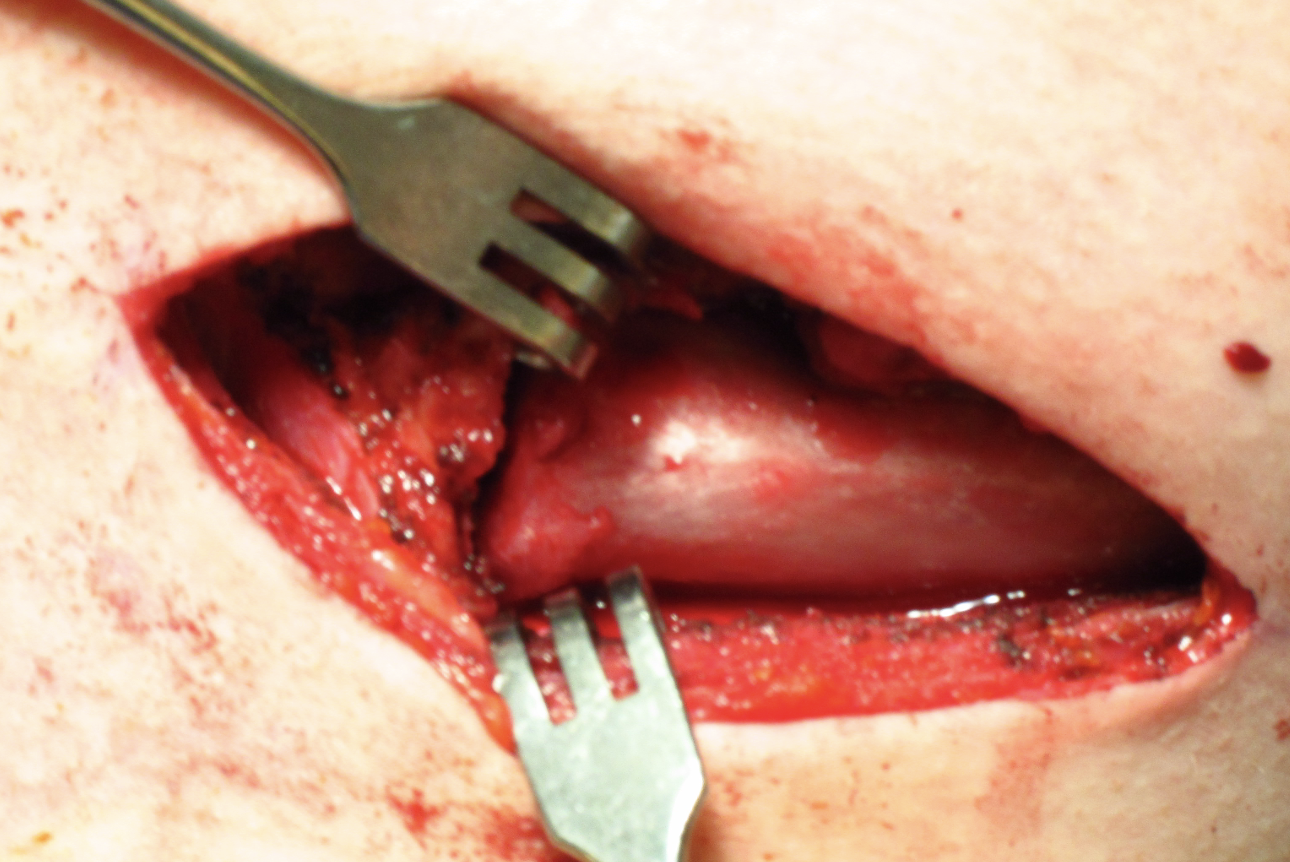
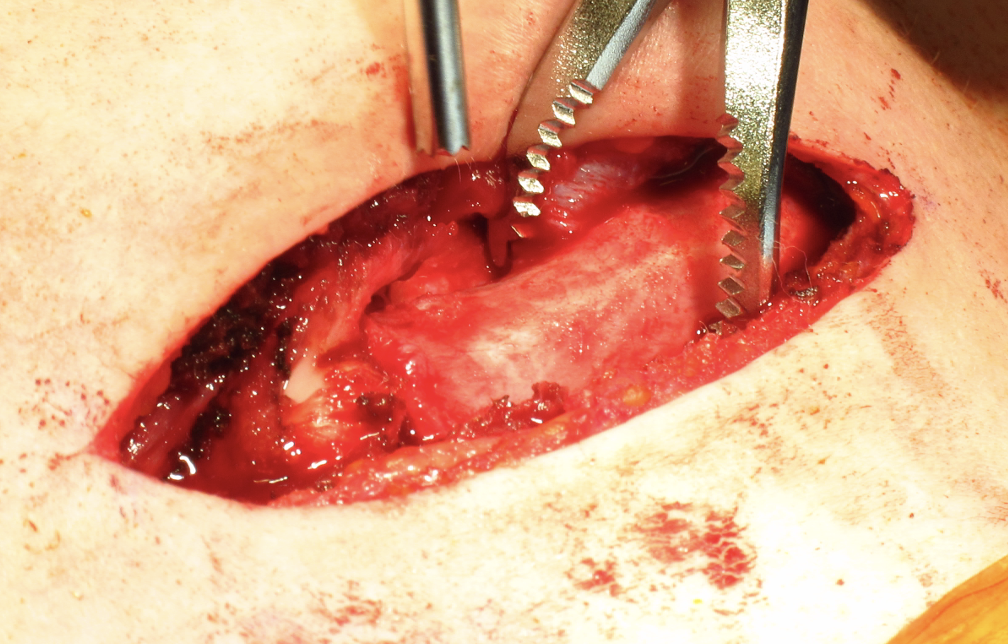
Open reduction of acute posterior sternoclavicular joint dislocation
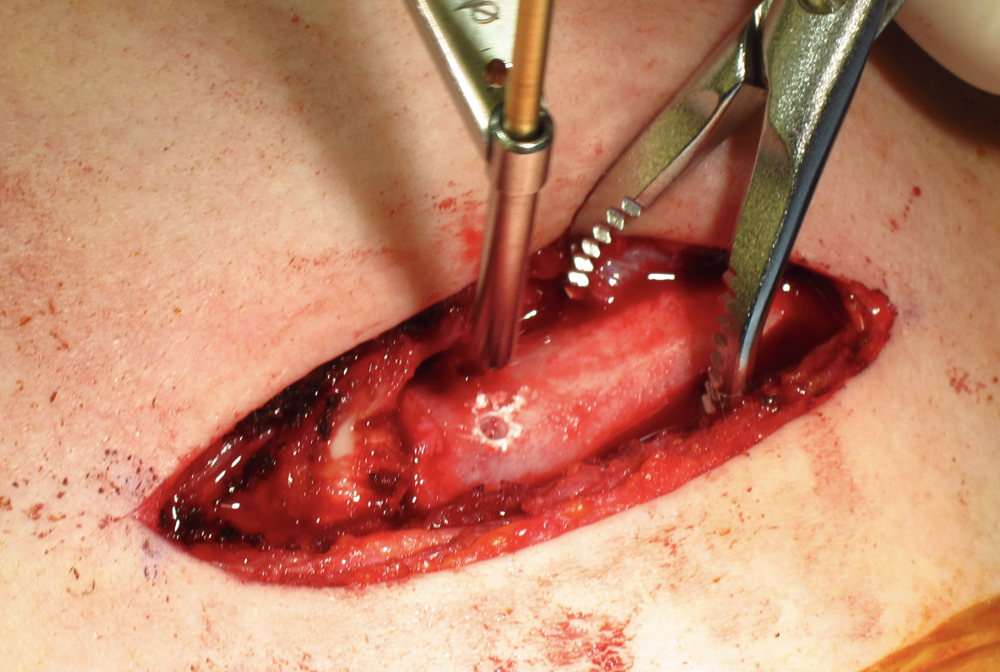
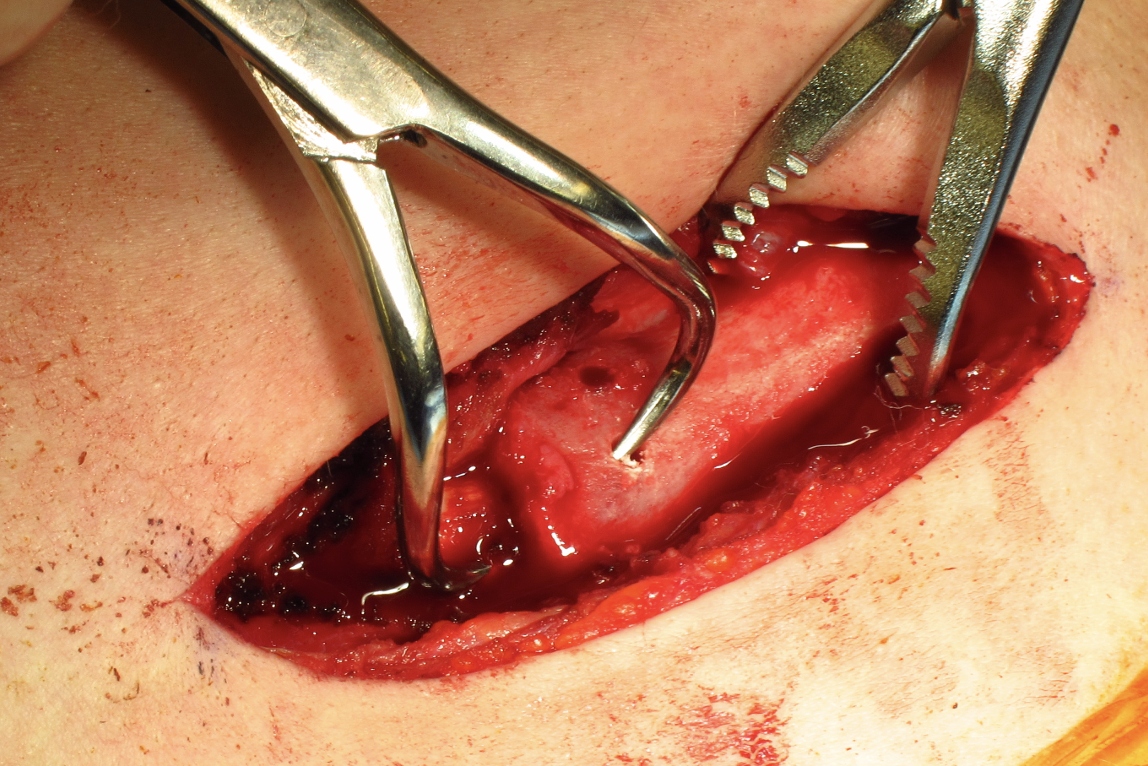
Drill holes in manubrium and medial clavicle
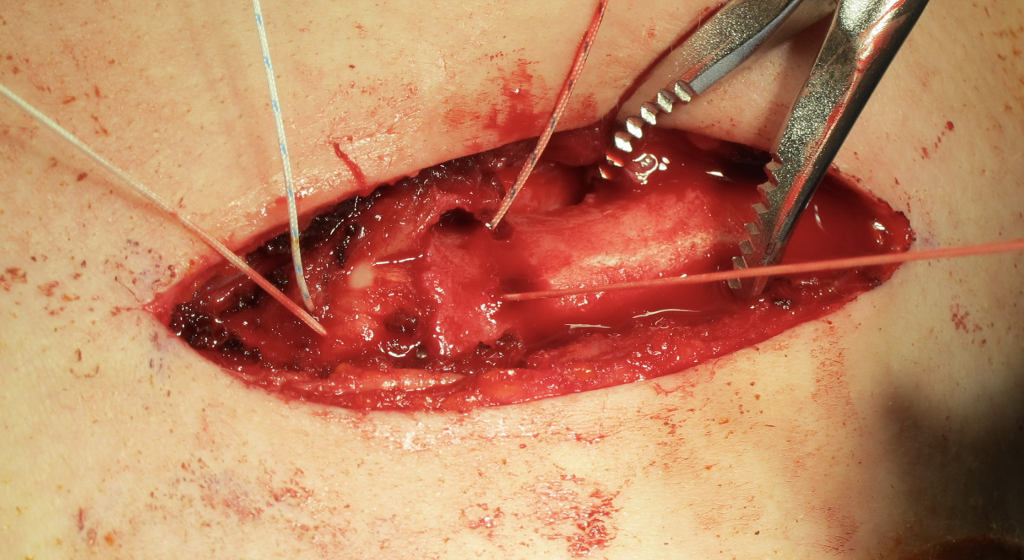
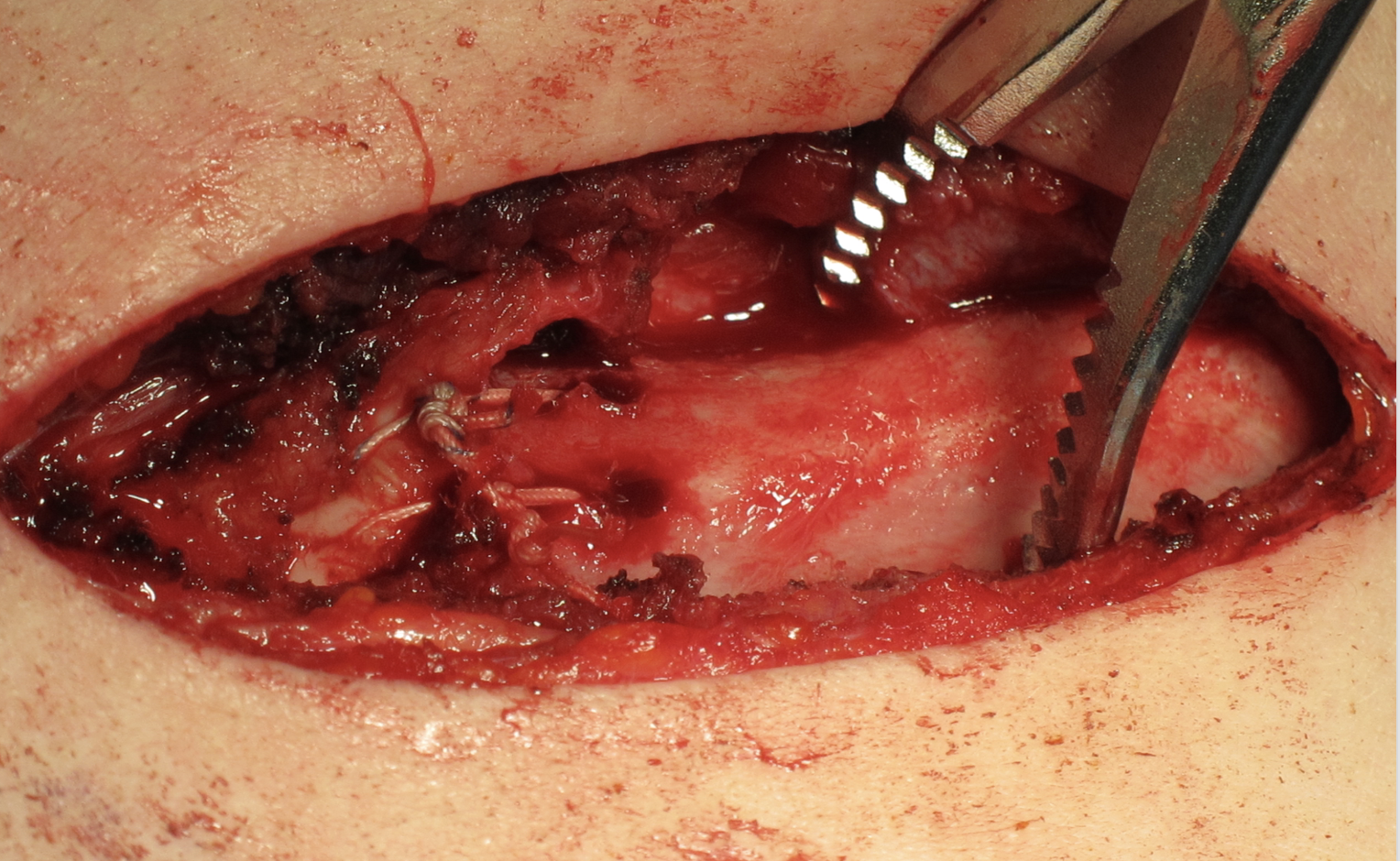
Figure of 8 suture fixation
Sternoclavicular joint septic arthritis
Presentation
Medial pain and swelling over 1 - 2 weeks
- predisposing factors: IVDU, diabetes, immunocompromised
- usually Staph aureus
Diagnosis
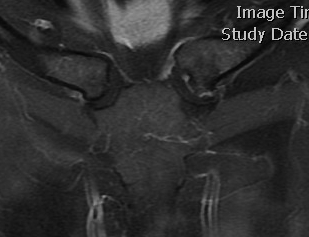
MRI - fluid / abscess
CT - bony erosions
Aspirate and culture
Management
- 170 cases of SCJ septic arthritis with mean age of 45
- 55% osteomyelitis, 25% chest wall abscess, 13% mediastinitis
- 50% Staph aureus
- 58% required surgical intervention (debridement +/- bony resection +/- soft tissue procedures)
Sternoclavicular osteoarthritis

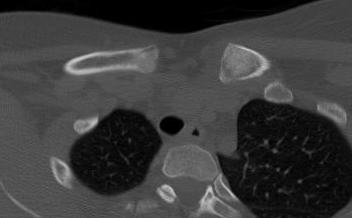
SCJ OA on the left with osteophytes and joint narrowing
Incidence
- 460 CT scans of SCJ
- 53% signs of asymptomatic OA
- 90% > 50 years old
- 100% > 60 years old
Associations
Can be symptomatic with rheumatoid and psoriatic arthritis
Options
Cortisone injection
Surgery
Open or arthroscopic medial clavicle excision
Vumedi open SCJ resection video
Vumedi arthroscopic SCJ resection video
SAPHO
Definition
Synovitis–acne–pustulosis–hyperostosis–osteitis (SAPHO)
- multiple osteoarticular and dermatological presentations
Pathogenesis
Unclear etiology
- combination of genetic / immunological / infectious
- managed by rheumatology and dermatology
Clinical
Middle aged women
- axial skeleton - SCJ, sterncostal joints, SIJ, vertebrae
- skin infections
- hips, knees, ankles
Imaging
Expanded bone / osteolysis / periosteal reaction
Elevated infection markers
Management
Immune modulators +/- antibiotics +/- bisphosphonates
Rarely surgical
Condensing Osteitis
Definition
Sclerosis of the medial end of the clavicle
Does not affect the sternum
Clinical
Local swelling and pain
Unilateral
Exclusively in women
Blood tests normal
Xray
CT
Management
Nonoperative
Natural history is to resolve over 6 - 12 months
Friedrich's Disease
Definition
Spontaneous osteonecrosis of medial end of clavicle
Management
Self limiting
Spontaneous resolution and remodelling occurs over 12 - 18 months
